Neonatology
Session: Neonatal General 7: Respiratory
245 - Current Continuous Positive Airway Pressure (CPAP) Use Among Premature Infants Admitted to the Neonatal Intensive Care Unit (NICU) Compared to a Historical Control: A Retrospective Chart Review
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 245
Publication Number: 245.2969
Publication Number: 245.2969

Anastasiya Latushko, MD (she/her/hers)
Fellow
Sidney Kimmel Medical College at Thomas Jefferson University/ChristianaCare/Nemours Children's Hospital DE
Wilmington, Delaware, United States
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) is associated with increased morbidity and mortality. The use of non-invasive respiratory support is one strategy to prevent BPD. It is unknown whether a gradual weaning strategy using high flow nasal cannula (HFNC) or the extended use of CPAP is superior. There was a perceived shift favoring the use of extended CPAP in our NICU after the initiation of a randomized controlled pilot study in 2022. It is unknown whether this shift is associated with improved outcomes.
Objective: To compare duration and weaning strategies as well as outcomes of infants born < 32 weeks’ gestation before and after a perceived change in practice favoring the use of extended CPAP.
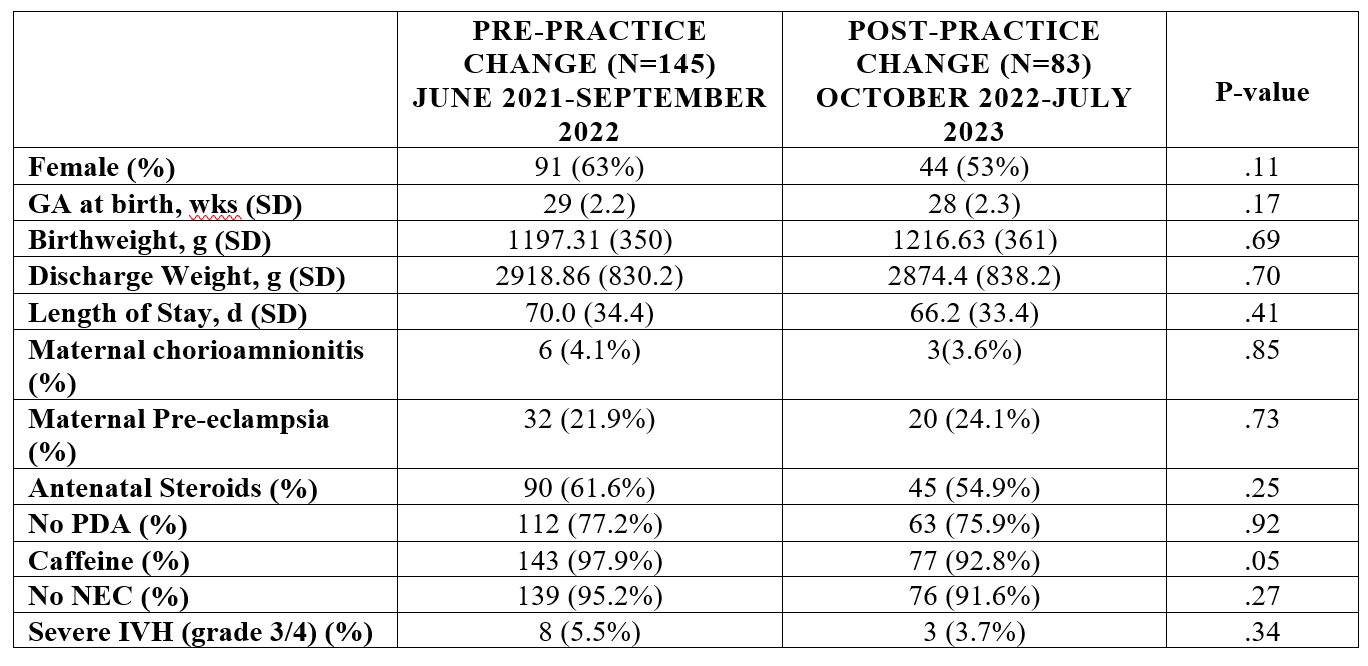
Design/Methods: This is a retrospective cohort study of infants born < 32 weeks in a single center NICU in Newark, Delaware. Starting in October 2022, infants were randomized to either extended CPAP use until at least 32 weeks corrected gestational age (CGA) or >1250g or to a gradual HFNC wean per unit standard. A chart review was conducted looking at infants born after October 1, 2022 compared to a historical cohort. The primary outcome was CGA to reach 2L or RA. Secondary outcomes included CGA to wean to each respiratory modality, rate of HFNC failure, CGA at discharge, feeding assessment, growth and incidence of BPD. BPD was defined by both VON and Jensen criteria.
Results: Interim analysis of 145 infants prior to the perceived practice change and 83 infants born after the perceived practice change was conducted. There was no significant difference in baseline characteristics (Table 1). Infants born after the perceived practice change were weaned to nasal cannula at an earlier CGA (33.6 ± 3.2 weeks vs. 32.8 ± 2.5 weeks, p=0.05), had less HFNC failure (29 infants (21.2%) vs. 8 infants (9.8%), p=0.03) and were discharged at an earlier CGA (39 ± 3.4 weeks vs. 38 ± 3.5 weeks, p=0.04) than controls. There was no difference in initiation of PO feeds, achievement of full oral feeds, or growth velocity. There was a trend towards less overall BPD per Jensen criteria among infants born after the practice change.
Conclusion(s): The use of extended CPAP in our unit may be associated with earlier weaning of non-invasive respiratory support and decreased BPD without increased morbidity. Data collection is ongoing.
.png)
