Neonatology
Session: Neonatal Neurology 1: Clinical
6 - Neurodevelopmental Outcomes of Infants Evaluated for but Not Treated with Therapeutic Hypothermia
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 6
Publication Number: 6.372
Publication Number: 6.372

Danielle Sharon, BS (she/her/hers)
Clinical Research Assistant
Brigham And Women's Hospital
Newton, Massachusetts, United States
Presenting Author(s)
Background: Therapeutic hypothermia (TH) is the standard of care for neonatal encephalopathy (NE). Although there is ongoing debate regarding the criteria for TH treatment, the criteria and protocol used in the Brigham and Women’s Hospital, which we have previously published, include infants with milder NE. Amplitude-integrated EEG (aEEG) is frequently incorporated into the evaluation. Whether these criteria, inclusive of mild encephalopathy, can screen out those with acute brain injury and adverse neurodevelopmental outcomes who might benefit from TH is unknown.
Objective: Our primary aim was to evaluate outcomes in a set of infants who were evaluated for TH but did not receive TH with neonatal MRI and 2-year developmental outcomes.
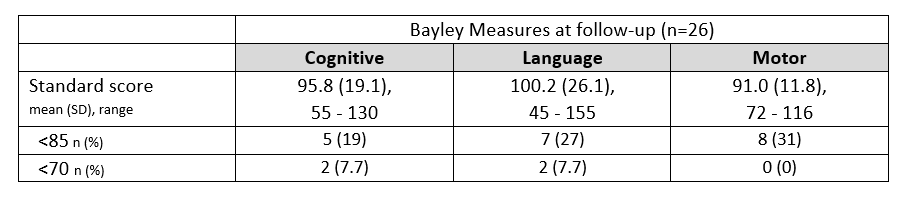
Design/Methods: We enrolled infants who were screened for but not treated with TH between April 2019 and August 2021. All brain MRIs were obtained within the first week of life. Infants were followed up at two years of age to obtain a standard Bayley-4 assessment conducted by a clinical psychologist. Neurodevelopmental delay was defined as any BSID-4 standard score < 85 (1 SD below mean).
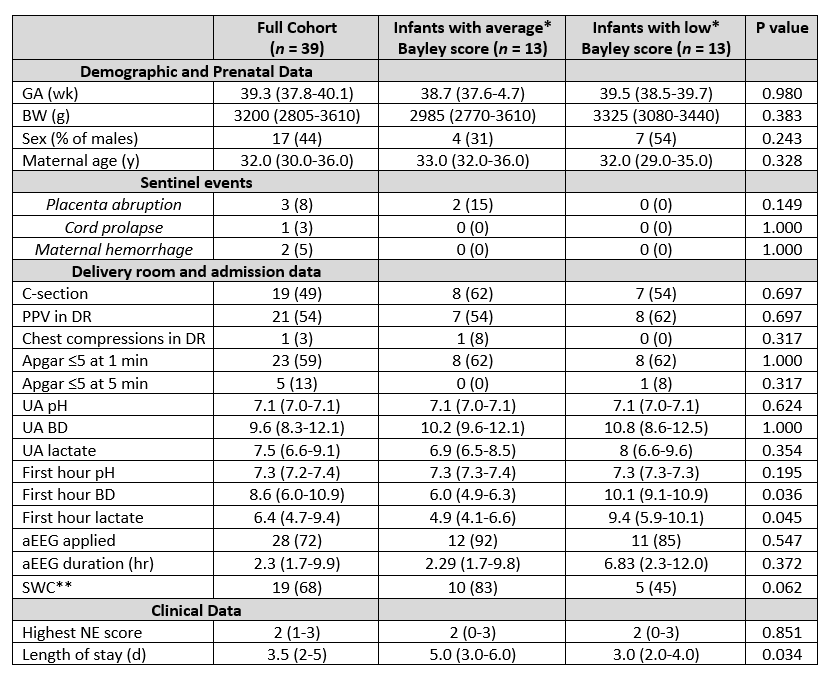
Results: Thirty-nine infants were enrolled in the study with their detailed demographic and clinical characteristics reported in Table 1. Of the 39 infants, 34 (87.2%) had no evidence of acute perinatally acquired hypoxic-ischemic brain injury (Thiim et al,2023). Twenty-six infants, three of whom had acute brain injury, returned for a 2-year follow-up Bayley-4 assessment. 13 (50%) had neurodevelopmental delay in either cognitive, language, or motor areas. Only one of the three infants with acute neonatal brain injury had neurodevelopmental delay. When compared to those without delay, infants with neurodevelopmental delay had higher 1-hour base deficit and higher lactate levels. Additional results from the Bayley assessments are in Table 2.
Conclusion(s): Results suggest that the current expanded TH criteria, inclusive of mild NE, is effective at detecting most infants with acute hypoxic-ischemic injuries. It is notable that a large percentage of these infants continue to be at risk for neurodevelopmental delay. Application of neuroimaging and neurodevelopmental follow-up in infants considered for hypothermia but not receiving treatment remains worthy of consideration. Whether recovery of blood gases can identify those with the highest risk needs further studying.