Emergency Medicine
Session: Emergency Medicine 4: Infections
106 - Are there risk factors associated with revisits to the emergency department in previously healthy children treated for croup?
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 106
Publication Number: 106.1607
Publication Number: 106.1607
Deanna Hano, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
The Children's Hospital at Montefiore
New York, New York, United States
Presenting Author(s)
Background: Croup can cause serious morbidity and mortality. Emergency department (ED) treatment pathways exist but there are occasionally treatment failures with patients revisiting the ED after discharge for similar or worsening symptoms.
Objective: To investigate patient-related and care-related factors associated with increased odds of ED revisits or subsequent hospitalizations within 3 days of ED discharge after treatment of croup.
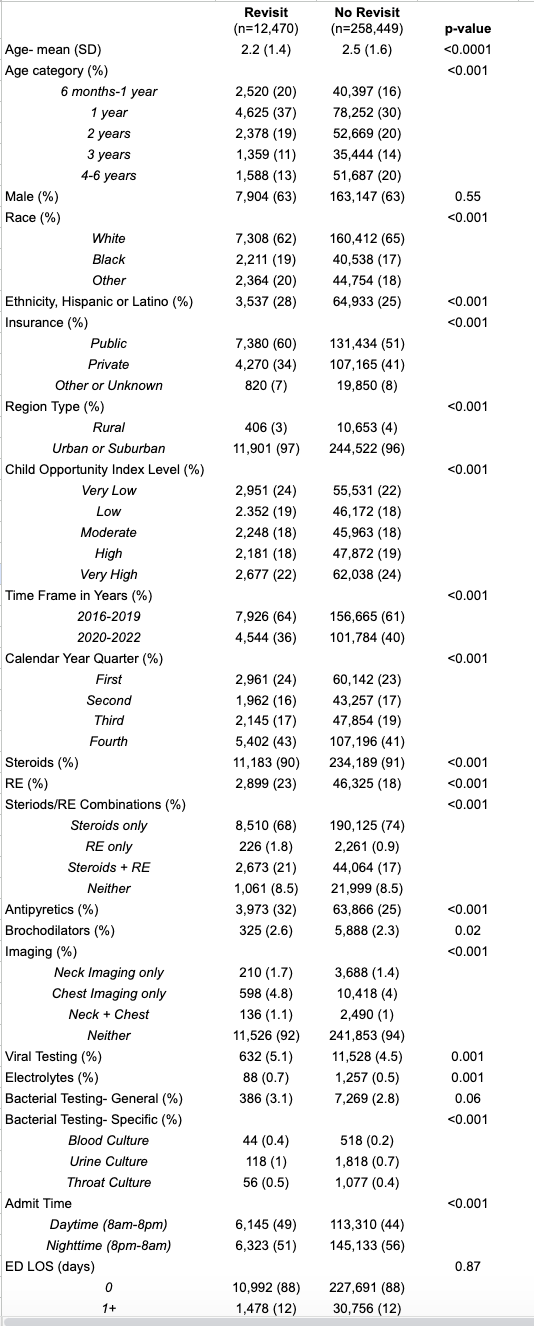
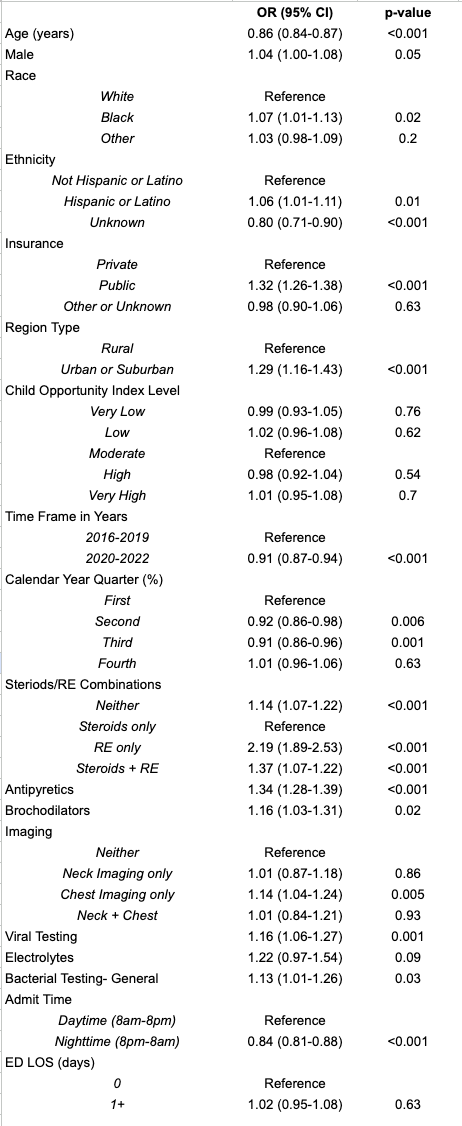
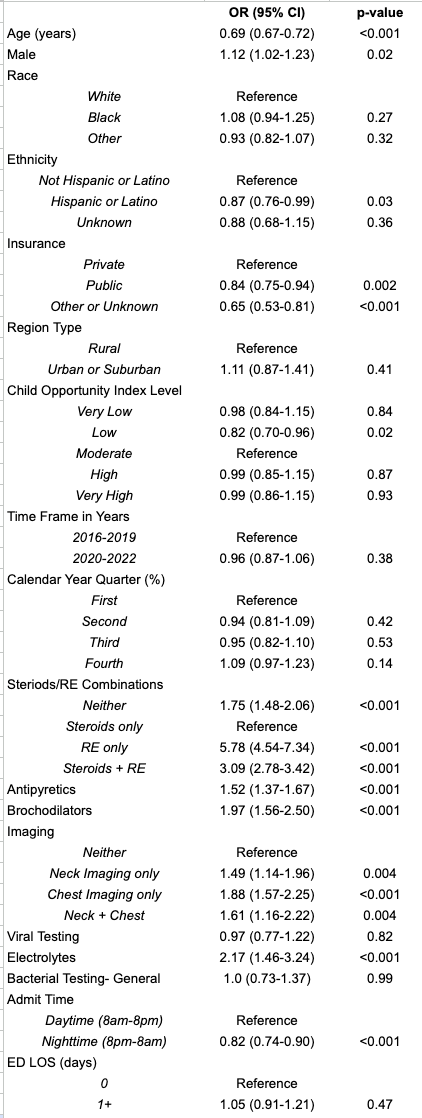
Design/Methods: This retrospective multi-centered cohort study utilizes Pediatric Health Information System (PHIS), a comprehensive database containing administrative data on ED and inpatient visits from 50+ participating pediatric hospitals. Previously healthy patients ages 6 months-6 years who presented to pediatric EDs between January 2016-December 2022 with a primary diagnosis of croup were included. Information on patient demographics, region, season, ED arrival time, ED medications administered, and ED laboratory analyses and imaging performed was collected. Characteristics of the revisit vs. non-revisit groups were compared using t-tests and chi-squared tests for continuous and categorical variables, respectively. Multivariate logistic regression analyses were used to evaluate the primary outcome (ED revisit within 3 days of discharge) and secondary outcome (hospital admission after an ED revisit).
Results: Of 270,919 unique croup patients seen and discharged from the ED, 12,470 (4.6%) revisited the ED within 3 days of discharge (Table 1). Compared to patients who did not revisit the ED, there were differences in patient- and care-related factors among those who revisited the ED and those who required subsequent admission (Tables 2 and 3). Patients who were younger, male, received antipyretics or bronchodilators, had chest imaging, and presented during the daytime had higher odds of revisiting the ED and subsequent admission. Compared to patients who received steroids alone, those who received racemic epinephrine (RE) alone or RE and steroids were more likely to return to the ED and require admission (OR 5.8 and 3.1, respectively).
Conclusion(s): This study found specific patient- and care-related factors associated with higher odds of ED revisits and need for subsequent admission, including receiving at least 1 dose of RE at an initial ED visit compared to receiving steroids only. Treatment may reflect severity of illness. These findings should prompt review of current ED guidelines with respect to the use of RE and discharge criteria, as well as consideration of other risk factors and severity of illness when deciding whether to discharge or admit a child with croup.