Emergency Medicine
Session: Emergency Medicine 11: Potpourri
416 - Racial Disparities in COVID-19 Infection and Outcomes Among Canadian Children Seeking Emergency Department Care: A Prospective Cohort Study
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 416
Publication Number: 416.3219
Publication Number: 416.3219

Gabrielle Freire, MDCM, MHSc (she/her/hers)
Emergency Physician
The Hospital for Sick Children
University of Toronto
Toronto, Ontario, Canada
Presenting Author(s)
Background: The exploration of known racial disparities in SARS-CoV-2 infection rates and subsequent outcomes among children is essential for equitable healthcare interventions. A nuanced understanding requires disaggregated racial data, currently lacking in large national datasets.
Objective: To determine the association between race and SARS-CoV-2 test positivity, interventions, hospitalization, and post-COVID conditions (PCC) in Canadian children.
Design/Methods: This is a secondary analysis of a prospective cohort study recruiting children < 18 years tested for SARS-CoV-2 at 14 Canadian pediatric emergency departments (ED), between August 2020 and February 2022. Demographic (age, sex, race), clinical (duration of symptoms, pre-existing conditions), and epidemiological risk factor (mask wearing, attendance at large gatherings or school/daycare) data was self-reported on questionnaire at the index visit. The primary outcome was SARS-CoV-2 test positivity. Secondary outcomes were interventions and hospitalization at or within 14 days of the index visit. PCCs were self-reported at 90-day follow-up. Associations between race and test positivity and interventions were tested using multivariable logistic regression models.
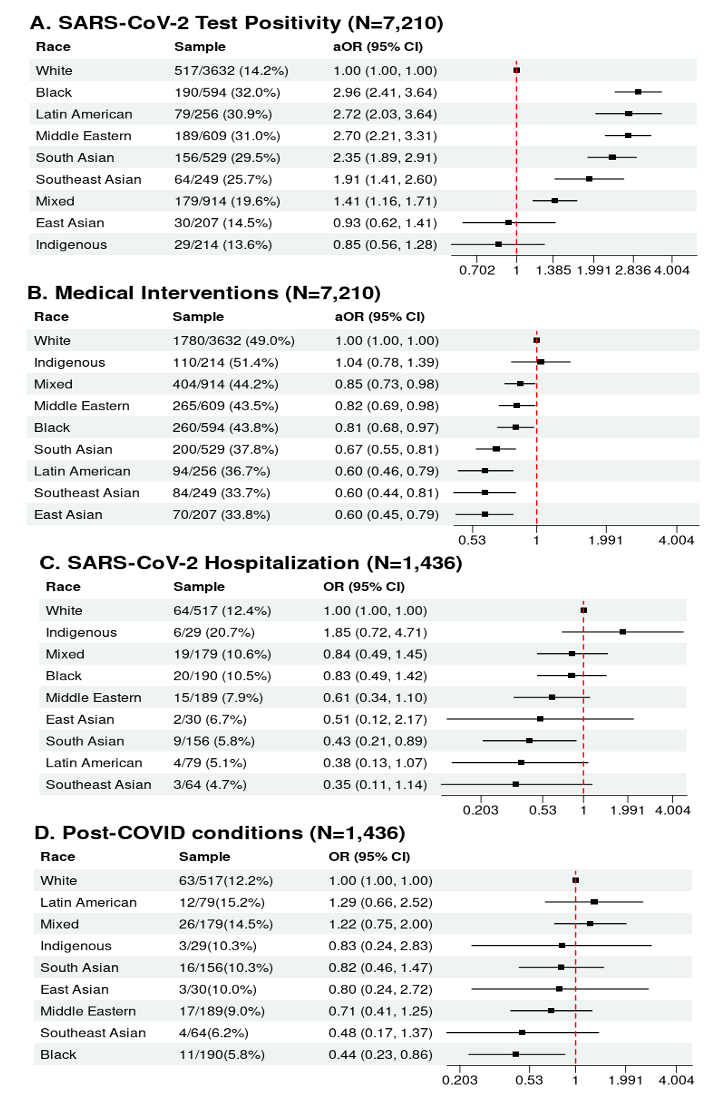
Results: We recruited 7293 children. Median age was 2.0 years (IQR: 1.0-5.0). 3,354 (47%) were female, and 1827 (25%) had a pre-existing condition. 1436 (20%) children tested positive for SARS-CoV-2, 636 (9%) were hospitalized, and 41 (0.6%) were admitted to an ICU. Compared to White children, most other racial groups were more likely to test positive for SARS-CoV-2 (aORs: Black 3.0 [95%CI 2.4-3.7], Latin American 2.8 [95%CI 2.1-3.7], Middle Eastern 2.7 [95%CI 2.2-3.3], South Asian 2.4 [95%CI 1.9-3.0], Southeast Asian 1.9 [95%CI 1.4-2.6], Mixed-Race 1.4 [95%CI 1.2-1.8], East Asian 0.9 [95%CI 0.6-1.4], Indigenous 0.9 [95%CI 0.6-1.3]). Children of all racialized groups other than Indigenous, had lower odds of interventions. Racial groups had similar odds of hospitalization and PCCs compared to White children, though South Asian children were less likely to be hospitalized (OR 0.4 [95%CI 0.2-0.9]) and Black children were less likely to report PCCs (OR 0.4 [95% CI 0.2-0.9]).
Conclusion(s): Our findings highlight racial disparities in SARS-CoV-2 test positivity and medical interventions among Canadian children in EDs, necessitating further research and advocacy efforts. A better understanding of the factors contributing to these differences will promote equitable healthcare across the population.