Neonatology
Session: Neonatal/Infant Resuscitation 2
276 - Differences in oxygen saturation and heart rate between late preterm and term newborn infants with delayed cord clamping in the first minutes after birth.
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 276
Publication Number: 276.3167
Publication Number: 276.3167
.jpeg.jpg)
Alvaro Solaz-García, Sr., RN, PhD (he/him/his)
Research Nurse
University and Polytechnic Hospital La Fe (HULAFE). Health Research Institute La Fe (IISLAFE).
Valencia, Comunidad Valenciana, Spain
Presenting Author(s)
Background: The fetal-to-neonatal transition is characterized by a series of physiological changes performed in an orderly sequence. Immediately after birth, the onset of breathing contributes to pulmonary vasodilatation thus enhancing gas alveolar-capillary gas exchange that causes a rapid increase the arterial partial pressure of oxygen. Deferring cord clamping (DCC) has been recommended by international guidelines and has become a standard of care world-wide. DCC contributes to hemodynamic stabilization and oxygenation of the newly born infant. Currently, no reference values for oxygen saturation (SpO2) and heart rate (HR) in the first minutes after birth for moderate and late preterm infants are available to support decision-making in the delivery room (DR).
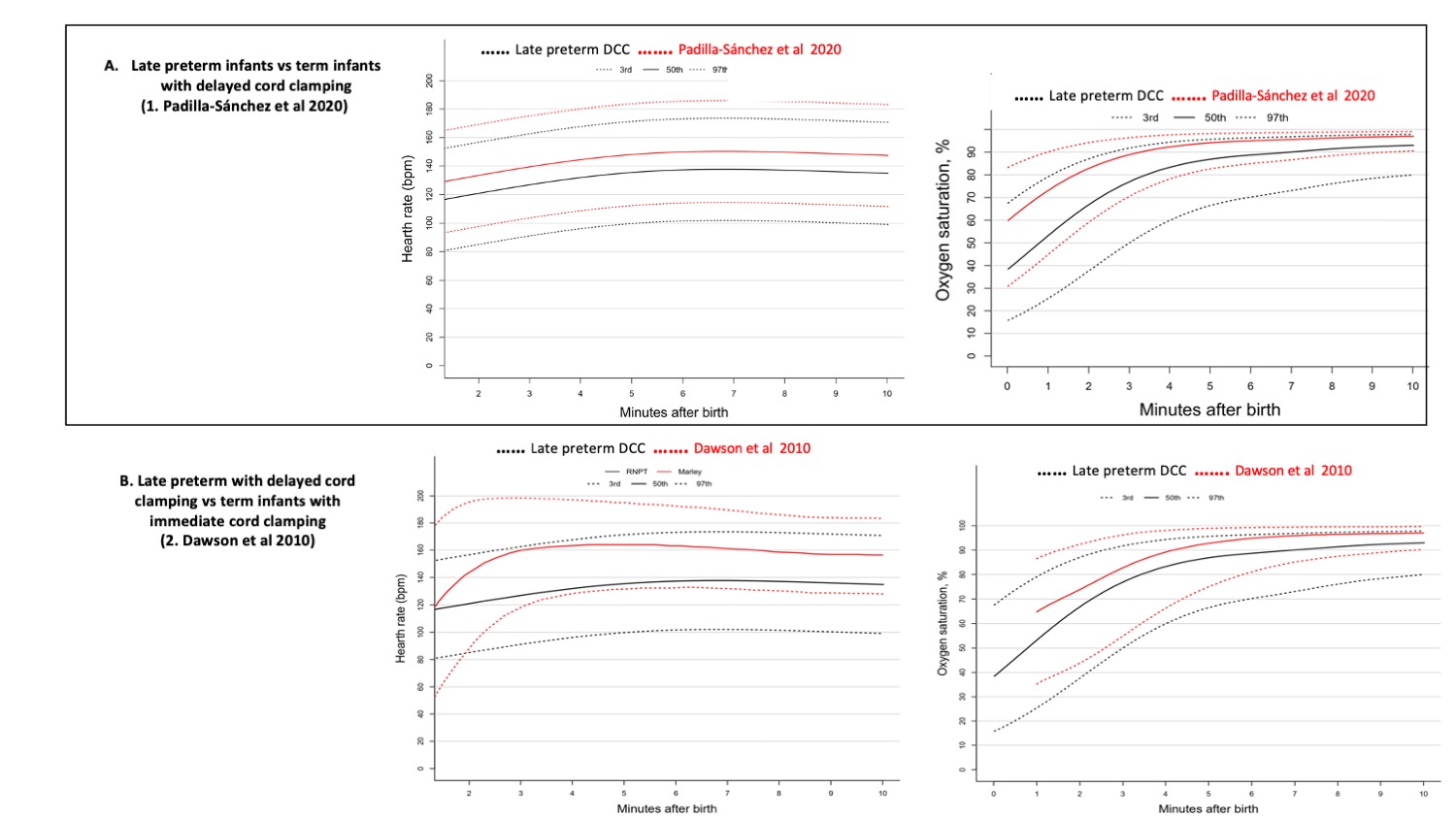
Objective: To build SpO2 and HR percentiles for the first 10 minutes after birth in late preterm infants born after an uneventful gestation subjected to DCC for > 30 seconds, and to compare with previously built percentiles for term newborns with and without DCC.
Design/Methods: This is a single-centre prospective observational study. Preductal SpO2, HR, timing of DCC, and temperature at the end of stabilization were recorded in late preterm infants between 32+0 to 36+6 weeks of gestational age born by vaginal delivery or C-section and who did not require resuscitation in the DR. The pulse-oximeter was adjusted in the right wrist/hand and set at maximal sensitivity and measurements performed every 2 seconds.
Results: A total of 96 late preterm infants were included. Median and IQR of gestational age was 34 (32-36) weeks. Median and IQR temperature at first 10 minutes after birth was 36.4ºC (35.7-36.8). Mean (SD) delay time for cord clamping was 70±27.1 seconds. The median and IQR of SpO2s at 3, 5 and 10 minutes after birth were 69% (58-75), 88% (82-92), and 95% (92-97), respectively. We found significantly lower SpO2 for the 10th, 50th, and 90th percentiles compared with the previous reference ranges for the first 5 minutes and HR for the first 4 minutes after birth. Figure 1 shows comparisons of the 10th, 50th, and 90th percentiles for SpO2 and HR in the first 10 minutes after birth in late preterm infants with previously published references ranges for term infants with and without deferred cord clamping considering that in the former only vaginal deliveries were included.
Conclusion(s): Spontaneously breathing late preterm newborn infants underwent DCC > 30 seconds achieved lower SpO2 and HR in the first 5 minutes and 4 minutes after birth, respectively, compared with term neonates born under the same conditions with and without immediate cord clamping.