Breastfeeding/Human Milk
Session: Breastfeeding/Human Milk 1: Breastfeeding
469 - Perceptions, Barriers, and Beliefs Related to Breastfeeding Among NICU Lactating Parents in Addis Ababa, Ethiopia
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 469
Publication Number: 469.1900
Publication Number: 469.1900

Gregory C. Valentine, MD, MED, FAAP (he/him/his)
Assistant Professor of Pediatrics, Division of Neonatology
University of Washington
Seattle, Washington, United States
Presenting Author(s)
Background: Early exclusive human milk (EHM) feeding is an evidence-based intervention to improve maternal-newborn-child health outcomes. In low-resource settings, parents lack lactation-supportive resources like breast pumps, milk storage options, and lactation specialists. Few studies have evaluated practices, perceptions, and barriers related to breastfeeding and lactation by mothers of newborns admitted to neonatal intensive care units (NICUs) in low-resourced settings.
Objective: To evaluate practices, perceptions, and barriers related to breastfeeding and lactation among mothers of babies in a tertiary referral hospital (St. Paul’s Hospital Millennium Medical College; SPHMMC) NICU in Addis Ababa, Ethiopia.
Design/Methods: We performed a mixed-methods convergent assessment including qualitative and quantitative survey-based questions distributed to mothers of newborns admitted to SPHMMC’s NICU. Descriptive statistics were utilized for demographic information from survey respondents; Fisher’s exact test evaluated knowledge and perception-related answers based on demographic categories.
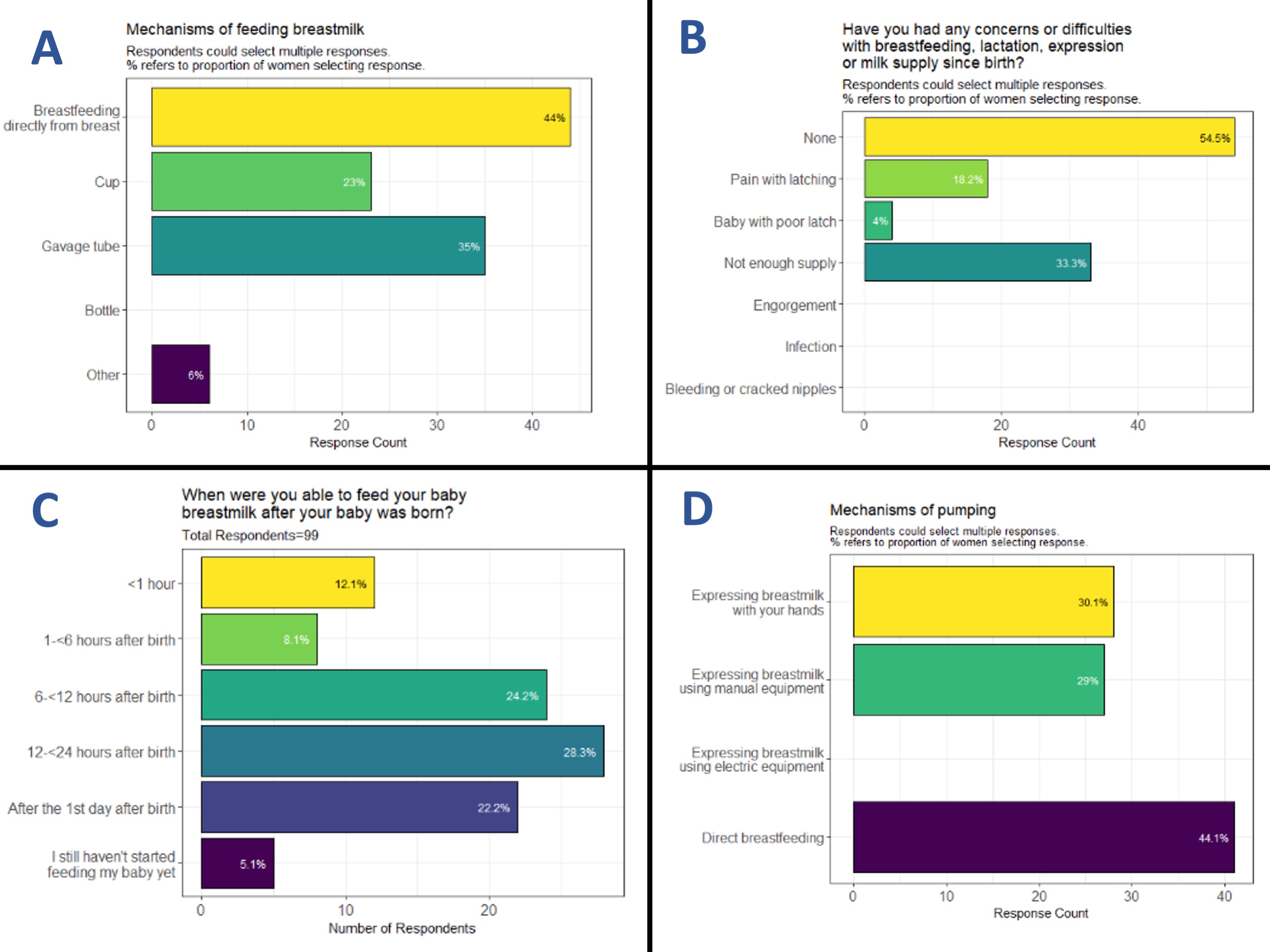
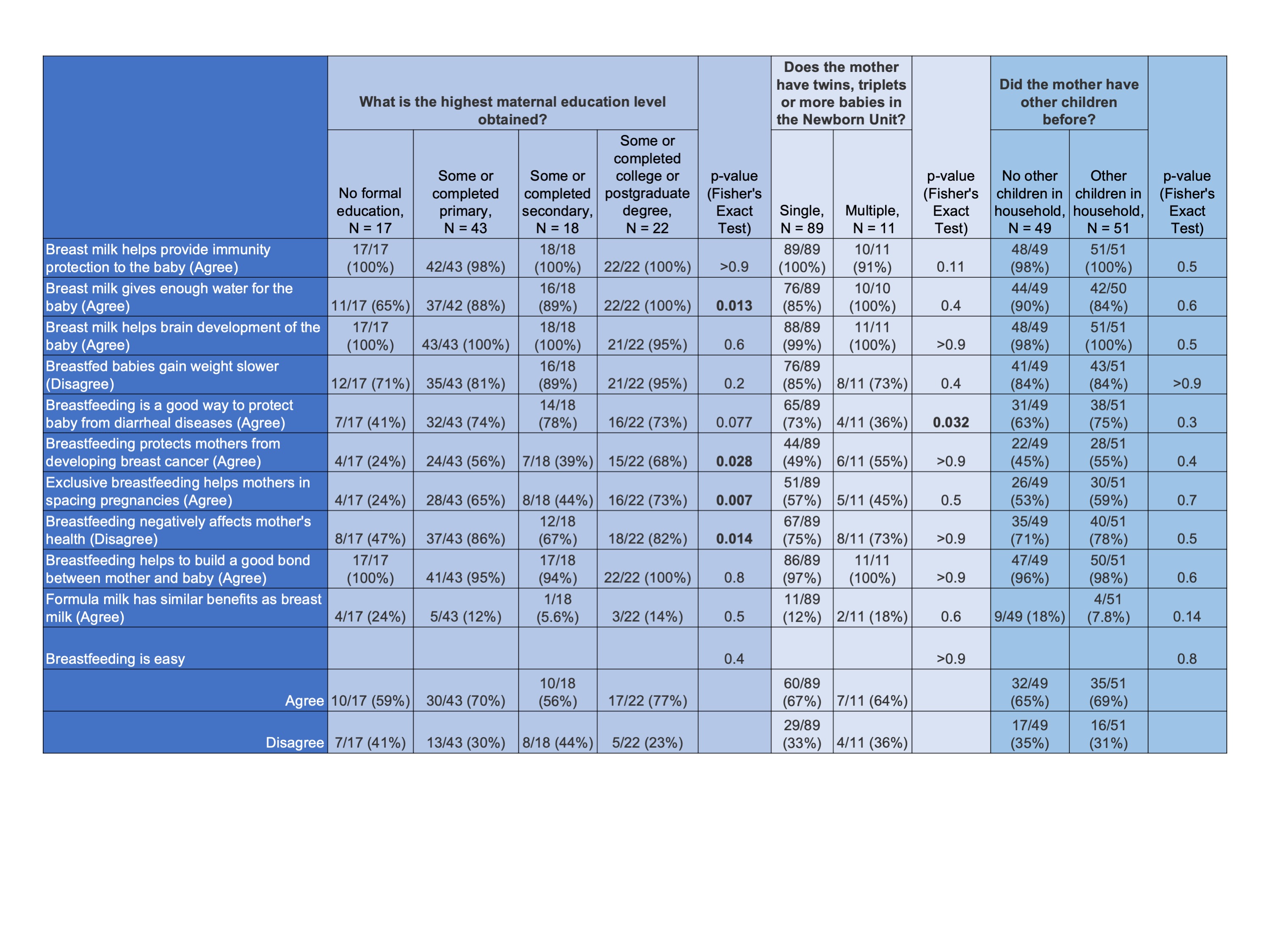
Results: Among n=100 mothers of NICU babies (Table 1), 94% (94/100) reported attempting to provide milk to their babies, and 79% hope to exclusively breastfeed after discharge. 72% of mothers do not have access to electric or manual pumps. >40% report having excess milk, of which 65% discard their excess milk. 9% of mothers said that if they are too sick, no one can transport milk to the NICU. 87% of mothers did not place baby to breast within the first hour after birth, and 55% newborns received first breastmilk after 12 hours (Figure 1). Compared with mothers of higher educational attainment, those without formal education had significantly lower understanding of maternal benefits of breastfeeding (i.e. reduced risk of future breast cancer (p=0.028), improved child spacing (p=0.007)), perceived breastfeeding as harmful to maternal health (p=0.014), and believed breast milk did not provide enough water for their baby (p=0.013; Table 2).
Conclusion(s): Despite goals for exclusive breastfeeding, SPHMMC NICU mothers do not have access to adequate resources to optimize lactation support and milk supply. When available, excess milk is simply discarded without access to storage materials or refrigeration. Mothers without formal education had less understanding of the maternal benefits to breastfeeding and also viewed breastmilk as not having enough water for newborns which may impact future care post discharge. Strengthening breastfeeding and lactation support programs at SPHMMC is imperative to improve maternal and newborn outcomes.
.png)