Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 2
371 - Strengthening Continuity of Care at an Academic Pediatric Primary Care Center through Quality Improvement Strategies
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 371
Publication Number: 371.1929
Publication Number: 371.1929

Alexandra M. S Corley, MD MPH FAAP (she/her/hers)
Assistant Professor
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Continuity of care, or the patient experience of seeing the same provider each visit, is prioritized by pediatric primary care centers and caregivers; continuity is associated with improved child health outcomes. A variety of challenges make continuity hard to achieve, especially in academic centers.
Objective: We sought to improve continuity in our pediatric academic primary care centers by implementing staggered interventions using quality improvement (QI) approaches.
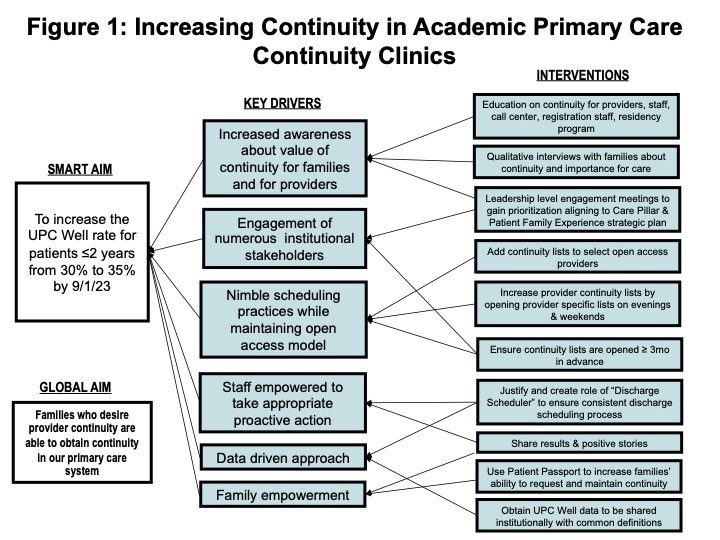
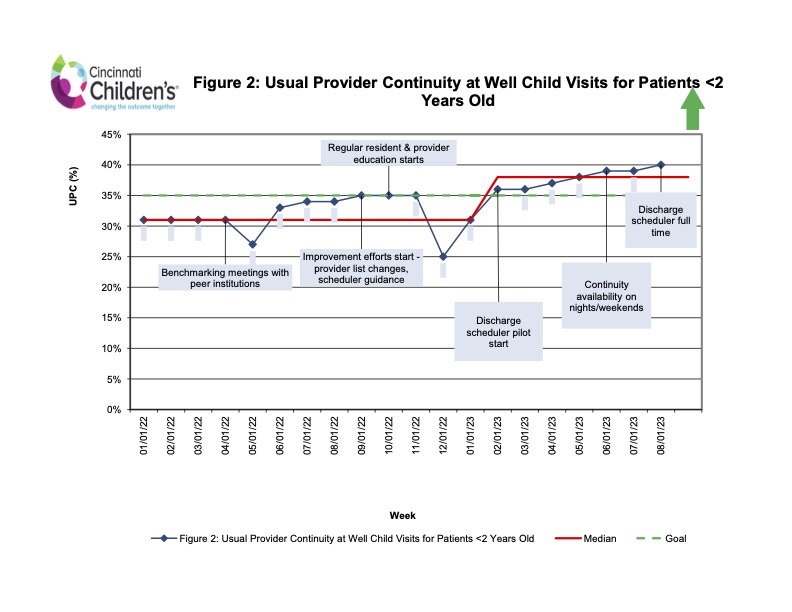
Design/Methods: We gathered baseline data of the usual provider continuity (UPC) rate at our largest academic primary care site, adjacent to the main hospital. There are 86 resident physicians at this site annually, alongside 23 attending physicians. The UPC is the number of visits with a “usual [continuity] provider” divided by the total number of visits. For our purposes, the usual provider was the provider with whom the patient had the most visits. We analyzed the median UPC for well child visits (WCVs) for children ≤2 years old. Failure modes informed the theory for improvement (Figure 1). Baseline data was collected 1/1/22-6/30/22; our intervention period was 7/1/22-9/1/23. We held benchmarking meetings with peer institutions to understand continuity barriers and approaches. We then completed several PDSA cycles for improvement; these included 1) scheduling improvements – provider availability changes and guidance for schedulers; continuity availability on nights and weekends 2) regular resident and attending provider continuity education and 3) establishing a novel role of Discharge Scheduler (DS) (Figure 2). The DS’s role has been modified since inception to best meet the needs of patients and families. Key collaborators in this improvement work have included departmental and divisional leadership, front line staff (scheduling center, nursing, and medical assistant colleagues), chief residents, and other educational leaders.
Results: Our baseline data revealed a median UPC rate of 31% for WCVs for children under 2 years old. After implementing the above scheduling, educational and support staff interventions, our center’s median UPC has improved to 38% for WCVs for children under 2 years old. This has resulted in an upward shift of the median line on our QI run chart (Figure 2).
Conclusion(s): QI efforts informing operational changes in a primary care setting—including enhancing provider availability, strengthening provider education, and creating new supportive staff roles—can help to improve provider-level continuity in academic settings with numerous providers.