Immunizations/Delivery
Session: Immunizations/Delivery 1
37 - Pediatric COVID-19 Vaccine Recommendation Practices, Attitudes, and Perceived Challenges in Rural Primary Care Providers
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 37
Publication Number: 37.1429
Publication Number: 37.1429

David Higgins, MD, MPH, MS (he/him/his)
Instructor of Pediatrics
University Of Colorado School Of Medicine
Centennial, Colorado, United States
Presenting Author(s)
Background: Pediatric COVID-19 vaccination rates lag drastically behind those of adults, especially in rural areas, due in part to parental vaccine hesitancy. A strong recommendation from a child’s primary care provider (PCP) is important for addressing parental vaccine hesitancy and one of the best predictors of vaccine uptake. The pediatric COVID-19 vaccine recommendation practices of rural PCPs have not been reported previously.
Objective: To describe, among rural PCPs in Colorado who routinely vaccinate children and adolescents, their pediatric COVID-19 vaccination: 1) recommendations compared to influenza and school-entry required vaccines; 2) attitudes; and 3) perceived challenges.
Design/Methods: From July to October 2023, a confidential survey was mailed and emailed to 326 PCPs in 17 rural Colorado counties listed in the Colorado Immunization Information System as vaccinating providers for patients < 18 years old. Fisher’s exact tests were used to compare strong recommendations for pediatric COVID-19, influenza, and school-entry required vaccines to all other recommendation types.
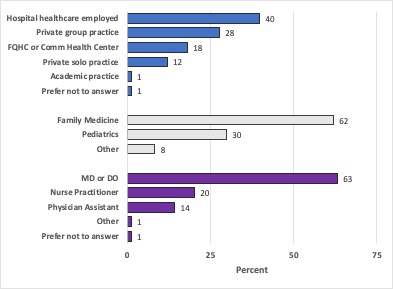
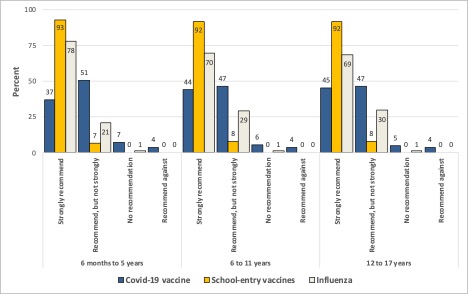
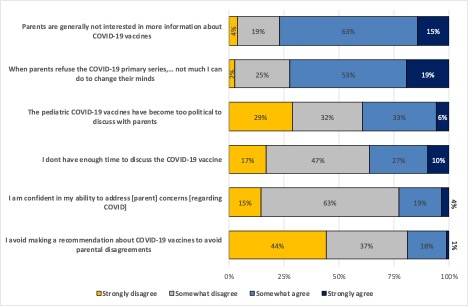
Results: There were 88 survey respondents (27% response rate): most were physicians (63%) and specialized in family medicine (62%) (Figure 1). For children 6 months – 5 years old, 37% of providers strongly recommended COVID-19 vaccines, compared to 78% for influenza (p=0.05) and 93% for school-entry required vaccines (p=0.08). For children 6 -11 and 12 – 17 years old, 44% and 45% of providers strongly recommended COVID-19 vaccines, respectively, compared to 69% and 70% for influenza vaccines (p < 0.001 for both age groups), and 92% for school-entry required vaccines (p=0.02 for both age groups) (Figure 2). Only 45% of providers strongly agreed that COVID-19 vaccines are important for their pediatric patients. The most common provider perceived challenges to discussing pediatric COVID-19 vaccines included a lack of parent interest in more information (78% “somewhat” or “strongly” agree), lack of ability to change parents’ minds (72%), and concerns the vaccines are too political (39%) (Figure 3).
Conclusion(s): Rural PCPs were less likely to make a strong recommendation for pediatric COVID-19 vaccines compared to influenza and school-entry required vaccines. Efforts to improve rural pediatric COVID-19 vaccine uptake through strong recommendations from PCPs should aim to increase provider vaccine confidence. Additionally, measures should address providers’ perceived pessimism regarding parents’ openness to vaccinate and concerns that COVID-19 vaccines are too political to discuss.