Emergency Medicine
Session: Emergency Medicine 9: Respiratory
233 - Implementation of an educational toolkit and incentive program is associated with decreased chest x-ray utilization for asthma, bronchiolitis and croup in a statewide emergency department network
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 233
Publication Number: 233.3213
Publication Number: 233.3213

John Greco, MD, PhD (he/him/his)
Pediatric Emergency Fellow
University of Michigan Medical School
Ann Arbor, Michigan, United States
Presenting Author(s)
Background: Approximately 10 million children present to emergency departments (EDs) annually for asthma, bronchiolitis, and croup (ABC). Decreasing routine chest X-ray (CXR) utilization in this population is part of the Pediatric ED Choosing Wisely campaign and consistent with national guidelines. The Michigan Emergency Department Improvement Collaborative (MEDIC) is an emergency physician-led network of over 40 EDs including general and pediatric hospitals. MEDIC maintains a clinical registry to track patient outcomes, identify best practices, and improve performance. MEDIC launched a quality improvement (QI) initiative in March 2019 to decrease routine CXR utilization in ABC patients. A subset of sites elected to use this CXR utilization metric as part of a pay-for-performance incentive model.
Objective: Analyze the impact of MEDIC’s QI initiative and incentive system on CXR utilization in patients diagnosed with asthma, bronchiolitis, or croup in a statewide network of EDs.
Design/Methods: We utilized International Classification of Diseases (ICD-10) codes to identify children less than 18 years old in the MEDIC registry with asthma, bronchiolitis, or croup from May 2017 to April 2023. The monthly rate of CXR utilization in these patients was calculated across all sites, and rates among incentive vs non-incentive sites were compared. Statistical process control charts tracked monthly CXR utilization and identified special cause variation. Admission rates and 72-hour ED return visits for a respiratory chief complaint were calculated as balancing measures.
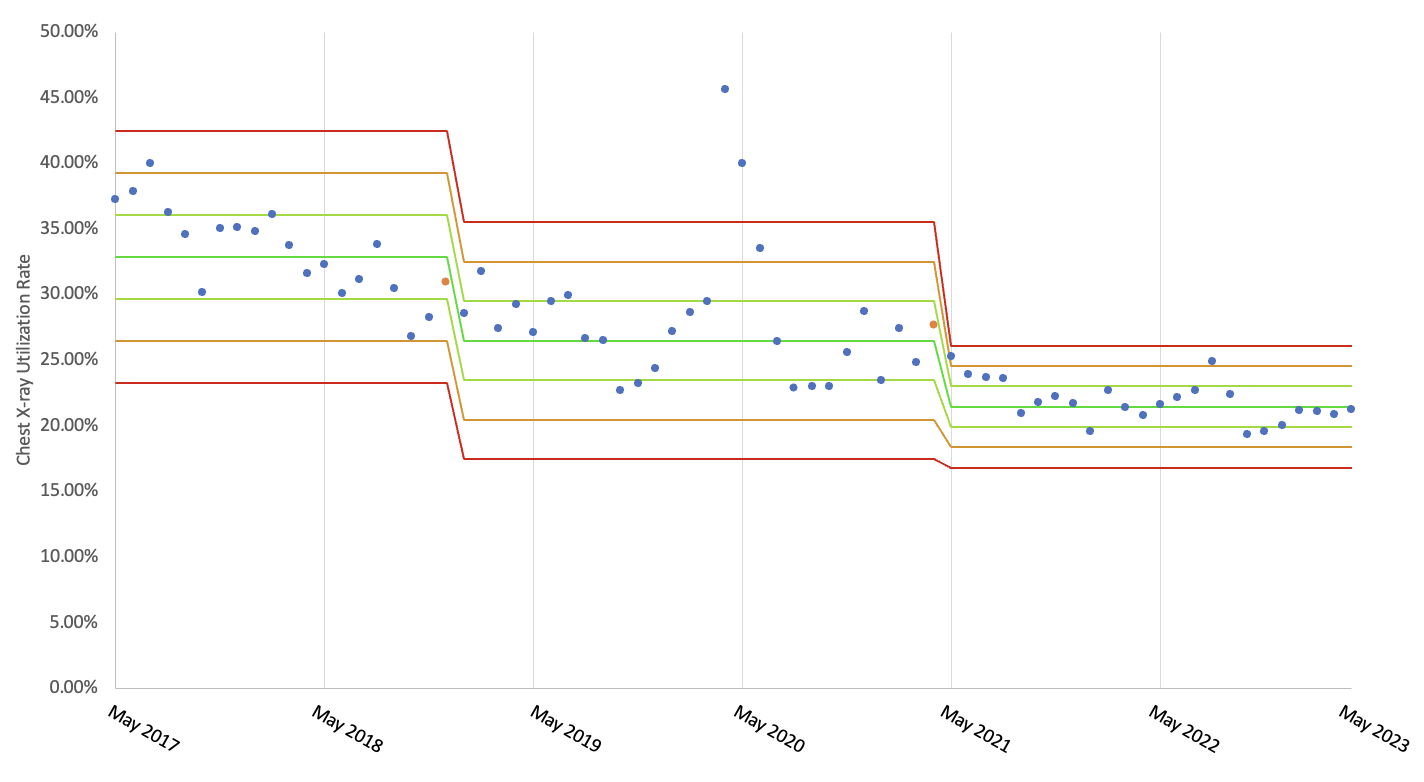
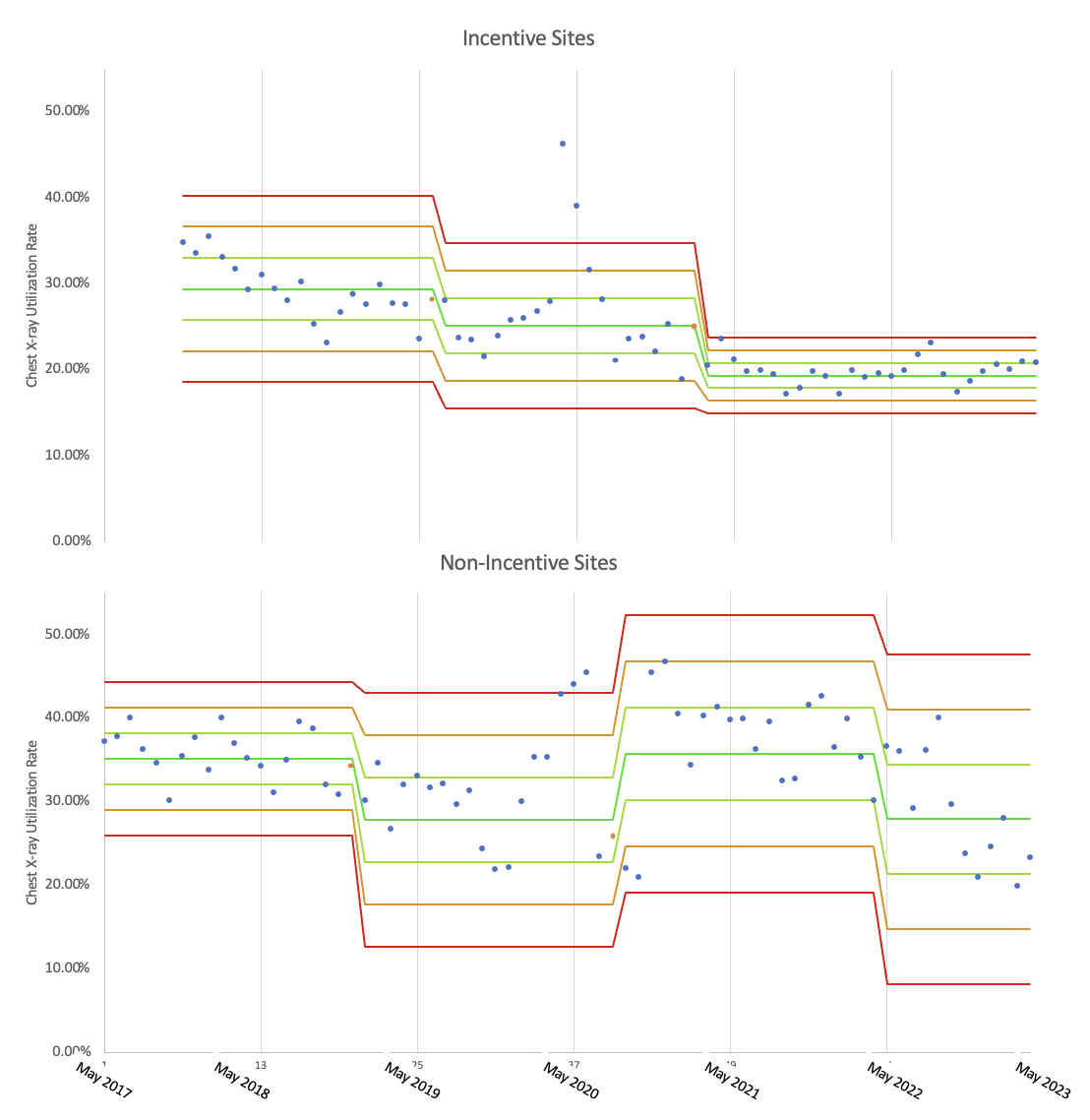
Results: There were 113,948 total ABC visits during the study period: 55,516 visits for asthma, 36,689 for bronchiolitis, and 26,330 for croup. CXR was obtained in 29.6% of patients with asthma, 31.1% of patients with bronchiolitis and 11.0% of patients with croup. Figure 1 demonstrates network-wide CXR utilization decreasing from 32.9% (SD=3.19%) to 21.45% (SD=1.55%). At incentive sites, CXR utilization decreased from 29.4% (SD=3.61%) to 19.3% (SD=1.46%), vs from 35.2% (SD=3.08%) to 27.9% (SD=6.57%) at non-incentive sites (Figure 2). For all ABC conditions, there was no significant change in admission rates and 72-hour ED revisit rates for respiratory chief complaints.
Conclusion(s): Implementation of this QI initiative was associated with a network-wide decrease in CXR utilization in patients with asthma, bronchiolitis, and croup without evidence of harm. Sites that were incentivized on CXR utilization had greater improvement than non-incentive sites during the study period, suggesting pay-for-performance incentive programs may support QI efforts.