Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 1: PDA
81 - Echocardiographic and Clinical Features of Spontaneously Closed Patent Ductus Arteriosus versus those requiring Treatment
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 81
Publication Number: 81.2017
Publication Number: 81.2017
.jpg)
Tatiana A. Nuzum, MB BCh BAO (she/her/hers)
Neonatal-Perinatal Medicine Fellow
Hassenfeld Children's Hospital at NYU Langone
New York, New York, United States
Presenting Author(s)
Background: Patent Ductus Arteriosus (PDA) is one of the most common complications of extreme prematurity, leading to neonatal morbidity and mortality. Prior research has struggled to define specific PDA features which should prompt treatment and, as a result, significant inter-institutional variability in terms of optimal management exists.
Objective: To evaluate whether a combination of early echocardiographic and clinical markers can predict whether PDAs will close spontaneously or require treatment.
Design/Methods: This was a retrospective review of neonates born less than 28 weeks GA at two Regional Perinatal Centers, NYU Hassenfeld and Bellevue Hospital NICUs, between 2018-2023 (n= 241). Subjects were excluded if they expired prior to echo, had other congenital heart disease or if echo results were unavailable (n=30). We collected results from subject’s first echo, and clinical data for entire NICU course. Subjects were stratified to study groups and compared based on whether PDA closed spontaneously or required active closure by means of medication, procedure or surgery. Statistical analyses included student’s t-test, Fisher’s exact test and Chi-Square.
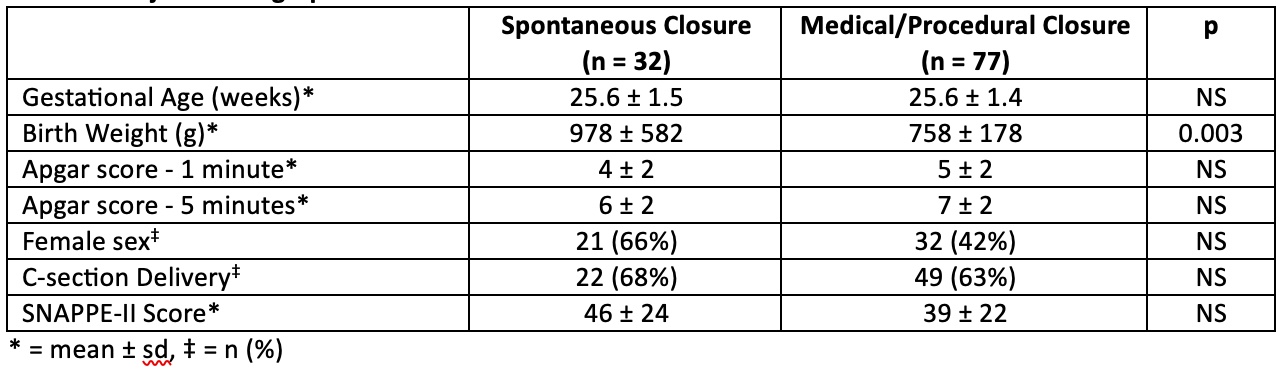
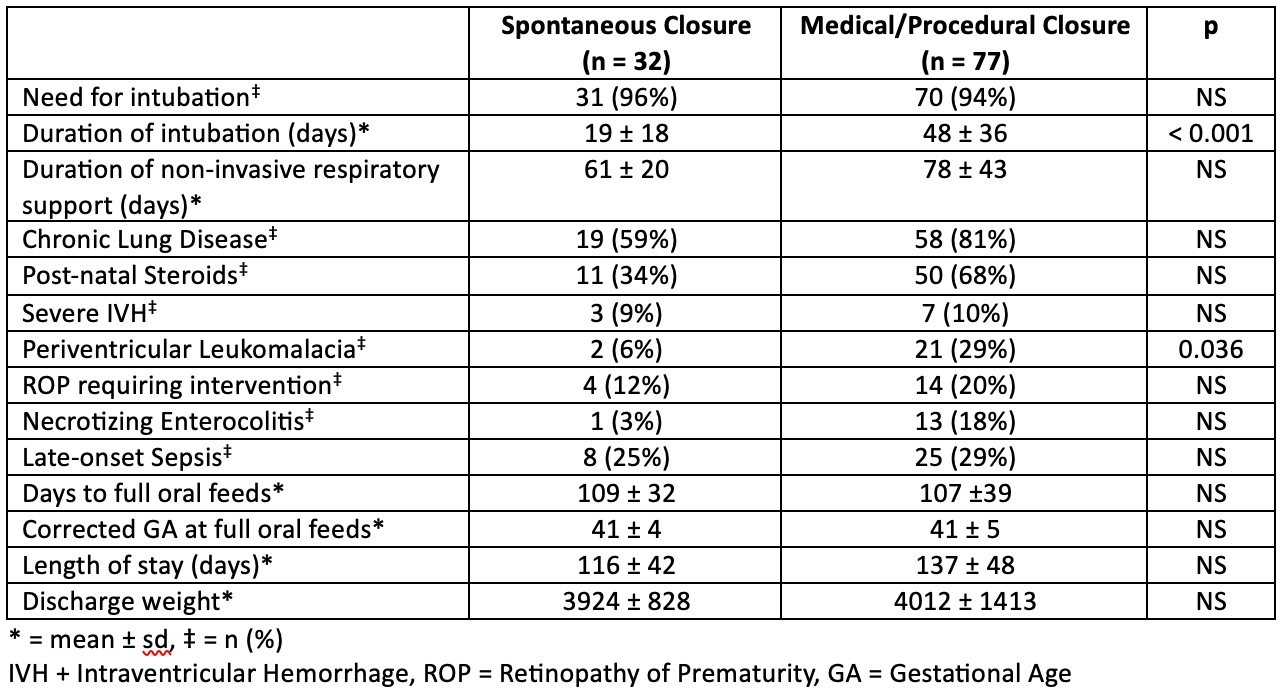
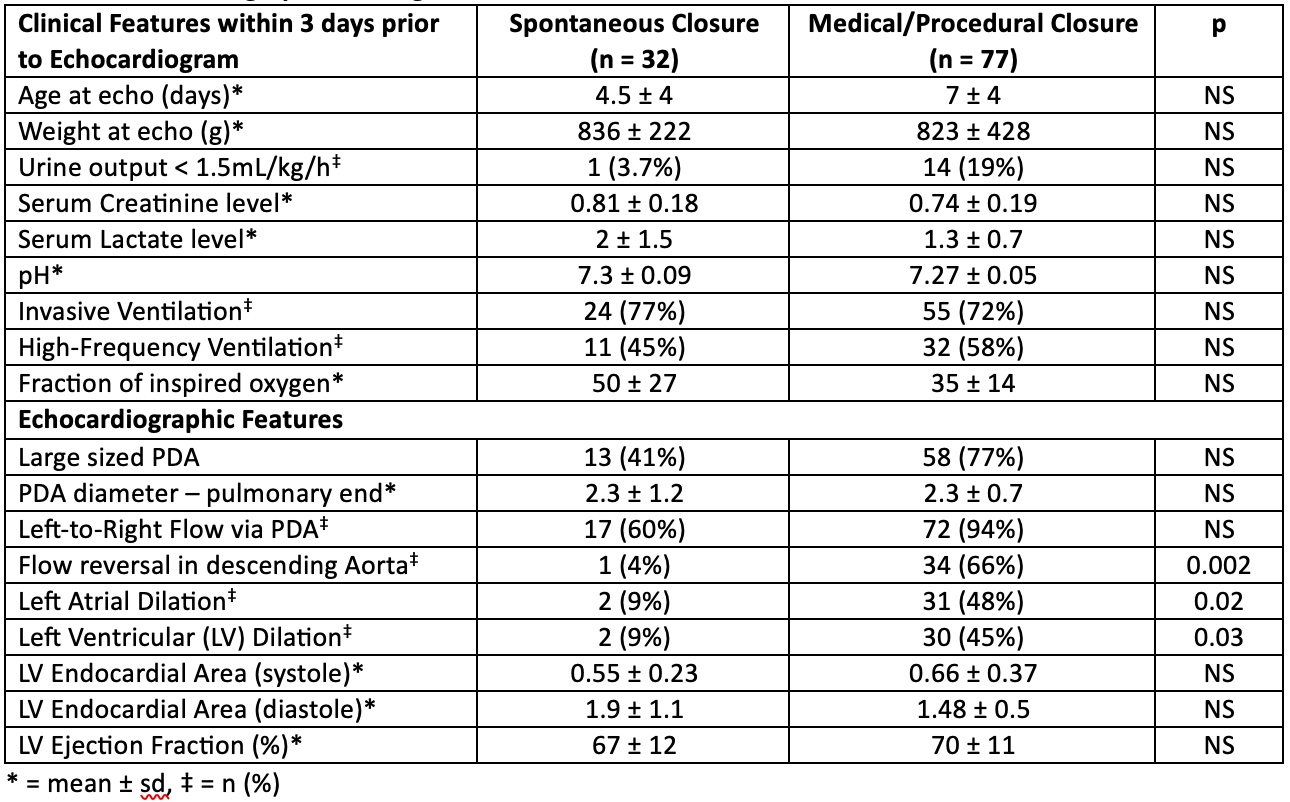
Results: PDA was diagnosed in 109/211 (51.7%) participants. There were 32 subjects in the spontaneous closure (SC) group, and 77 that underwent active closure (AC). Subjects in the SC group had significantly higher birth weights (978 v 758g, p = 0.003) (Table 1), although there were no other significant baseline differences between groups. Subjects who underwent AC required invasive respiratory support for longer (48 v 19 days, p < 0.001) and had higher rates of Periventricular Leukomalacia (29% v 6%, p = 0.036) (Table 2). Age and weight at time of echo was similar between groups (Table 3). There were no significant differences in various clinical parameters within 3 days of echo including pH, lactate, urine output and ventilatory requirements. There was no difference in PDA size or diameter between groups. Subjects in the SC group were less likely to have descending aorta flow reversal (4% v 66%, p = 0.002), left atrial dilation (9% v 48%, p = 0.02) and left ventricular dilation (9% v 45%, p = 0.03) as compared to the AC group.
Conclusion(s): Smaller neonates were less likely to undergo spontaneous PDA closure. Effects of hemodynamic significance, rather than size or diameter of PDA, proved to more reliable predictors of PDA course. Comprehensive echocardiographic assessments should pay close attention to these features. Future directions will include further investigation as to whether these metrics can also predict response to different treatment options.