Neonatology
Session: Neonatal Pulmonology - Clinical Science 1: BPD, BPD Biomarkers and Diagnosis
187 - Preeclampsia alters the inflammasome component profiles of tracheal aspirate fluid in extremely premature infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 187
Publication Number: 187.3058
Publication Number: 187.3058
- VC
Veronica Caballero, MD
Fellow
Holtz Children's Hospital Jackson Memorial Hospital
Miami Springs, Florida, United States
Presenting Author(s)
Background: PE is associated with a pro-inflammatory intrauterine state but its persistence in the preterm lung after birth has not been determined. Inflammasomes are multi-protein complexes that activate caspase-1 leading to programmed cell death and inflammation. Apoptosis-associated speck-like protein containing a caspase recruitment domain (ASC) is pivotal in inflammasome assembly and activation of caspase-1.
Objective: To determine if PE is associated with alterations in the inflammasome activation component profiles, specifically caspase-1 and ASC, in the tracheal aspirate fluid (TAF) in preterm infants.
Design/Methods: TAF was collected at postnatal day 7 from intubated infants born at 23-28 weeks gestational age, admitted to the NICU at Holtz Children’s Hospital of the University of Miami/Jackson Memorial Medical Center. Inflammasome components were measured by Ella Simple Plex and normalized to protein concentration. The relationship between PE and inflammasome profiles was examined using Generalized Linear Models adjusting for gestational age. Analysis done by Mann Whitney U Test.
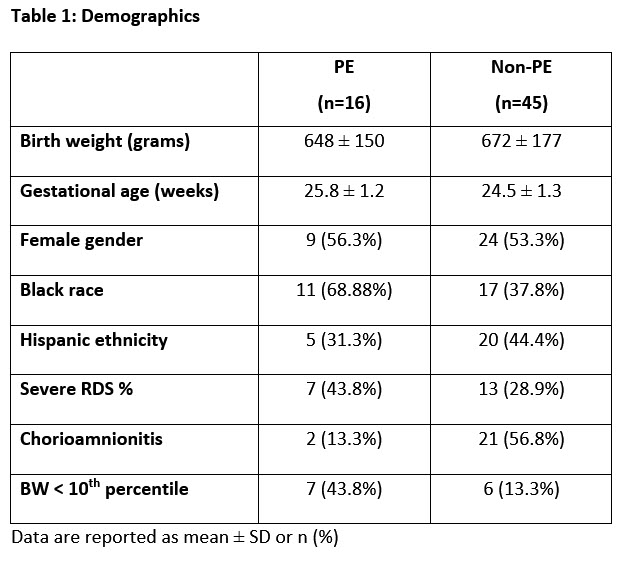
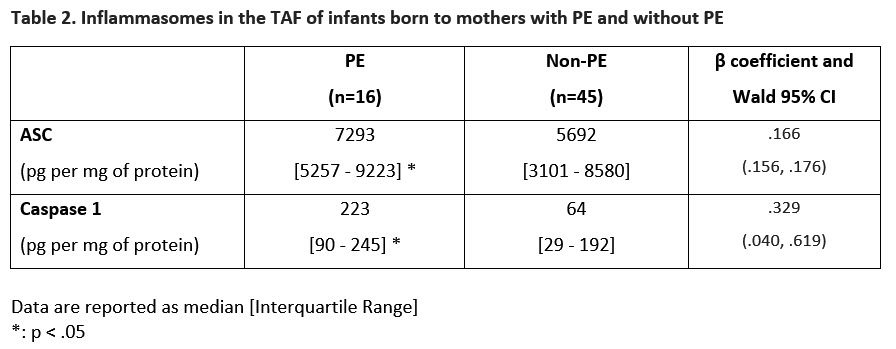
Results: The cohort included 61 preterm infants of whom 16 were born to mothers with PE. Demographics are shown in Table 1. Infants born to mothers with PE had significantly higher caspase-1 and ASC levels in the TAF compared to non-PE infants (Table 2). Analysis by Generalized Linear Models showed increasing ASC levels and caspase-1 log were associated with PE after adjustment for gestational age.
Conclusion(s): In this cohort of extremely preterm infants, PE was associated with increased caspase-1 and ASC levels in the TAF. This suggests the persistence of the pro-inflammatory profile that involves inflammasome activation in the lungs of preterm infants during the early postnatal period. The impact of these alterations on lung development needs to be examined.
(Supported by NHLBI grants U01 HL133689, UO1 HL133708, R01HL156803).