Emergency Medicine
Session: Emergency Medicine 1: Operations and Research
364 - Pediatric Readiness Score and Potentially Avoidable Transfers: A Single Center Experience
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 364
Publication Number: 364.470
Publication Number: 364.470

Kristen Capito, DO (she/her/hers)
Pediatric Emergency Medicine fellow
Le Bonheur Children's Hospital/UTHSC- Memphis
Memphis, Tennessee, United States
Presenting Author(s)
Background: Based on prior studies, 20-40% of transferred pediatric patients are discharged directly from tertiary Emergency Departments without requiring specialized intervention. Avoidable transfers can impose burdens on patients and families with duplicated tests, increased possibility of inpatient admission, and increased costs and stress related to travel and lodging. Most pediatric patients seek emergency care in local community hospitals which may not be equipped to handle pediatric cases necessitating transfers. The National Pediatric Readiness Project (NPRP) assesses the readiness of emergency departments (EDs) in treating pediatric patients with scores based on criteria outlined in the 2009 “Guidelines for Care of Children in the Emergency Department.”
Le Bonheur Children’s Hospital is a pediatric tertiary care facility serving a 3-state catchment and the only level 1 trauma center in the region. As such, Le Bonheur receives a large number of transfers from small community EDs. To date, there are few studies analyzing the relationship of pediatric readiness scores and referrals to higher level of care institutions.
Objective: To determine if weighted pediatric readiness scores (WPRSs) from NPRP 2021 survey are associated with potentially avoidable transfers (PATs).
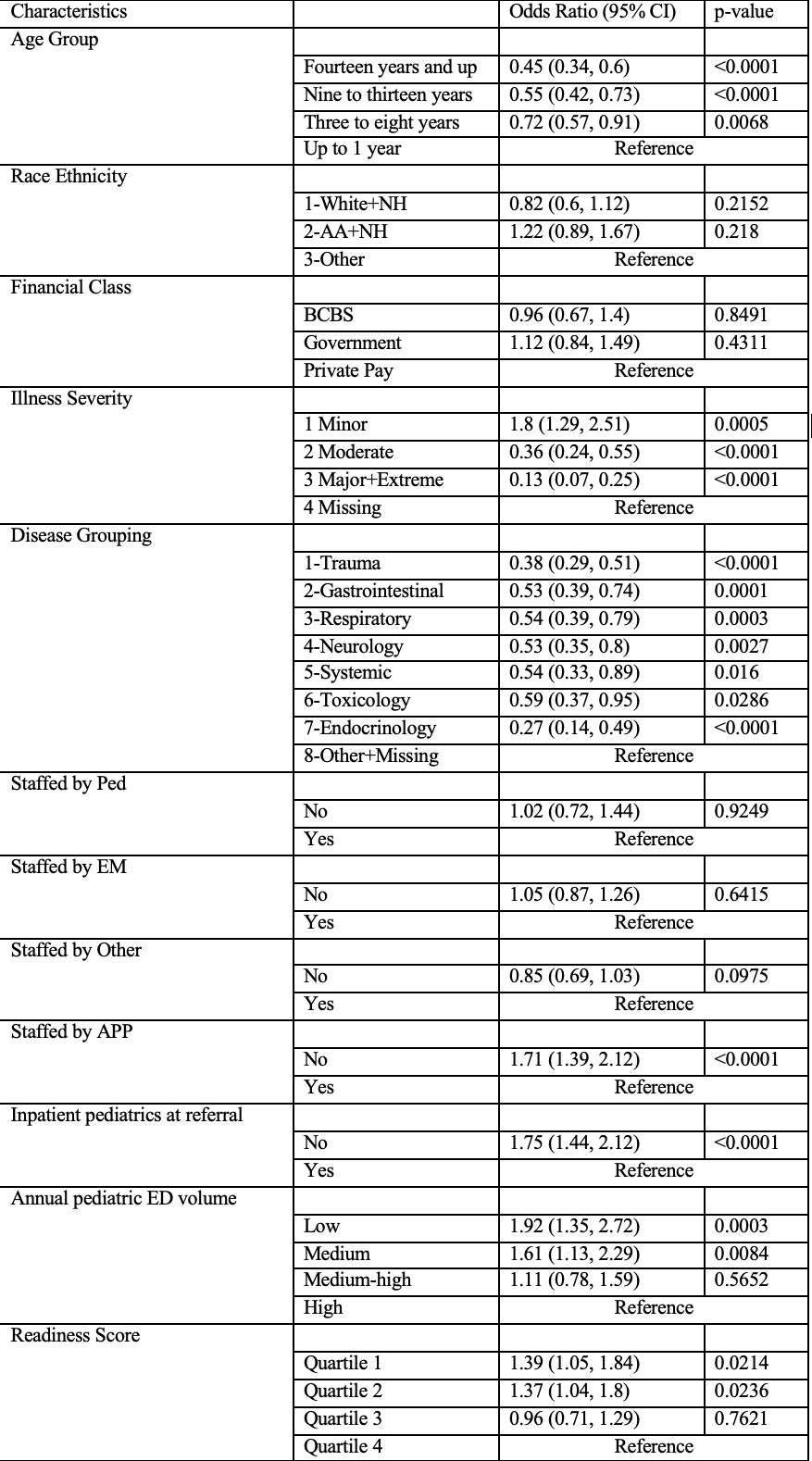
Design/Methods: This retrospective, observational study examined patient and hospital-level characteristics of all patients transferred to Le Bonheur from outlying EDs in 2021. Pediatric readiness was assessed using the 2021 WPRSs of the referring hospital. PATs were defined as patients who did not require admission, procedural sedation, or in-person specialist consultation. The relationship between hospital-specific pediatric readiness and PAT encounters was evaluated using multivariable logistic regression.
Results: We studied 2,338 patient transfers from 107 outlying EDs. The median WPRS was 78.5 (range, 42.2–100). Univariate analysis showed that PATs were associated with older patients, milder disease severity, lack of inpatient pediatrics at referring facility and low/medium annual pediatric ED volume. Adjusting for age, illness severity, disease grouping, and staffing, presentation to a hospital in the lowest readiness quartile was associated with increased odds of a potentially avoidable transfer (adjusted odds ratio compared to the highest quartile, 1.51; 95% confidence interval, 1.11–2.05; P < 0.008).
Conclusion(s): Presentation to hospitals with lower WPRSs was significantly associated with greater numbers of potentially avoidable transfers.
.png)
.png)
