Neonatology
Session: Neonatal General 9: Outcomes, Genetics. Ethics
384 - Bradycardia Recognition and Detection in Young Infants (BRADY-I Study): The Diagnostic Accuracy of a Commercial Home Cardiorespiratory Infant Monitor
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 384
Publication Number: 384.2763
Publication Number: 384.2763

Colm P. Travers, MD (he/him/his)
Assistant Professor
University of Alabama School of Medicine
Birmingham, Alabama, United States
Presenting Author(s)
Background: The diagnostic accuracy of commercially available home monitors in infants at high risk of cardiorespiratory events is not known and there are concerns about false alarms.
Objective: To determine the diagnostic accuracy of the Owlet OSS 3.0 (Owlet, Lehi, UT) for cardiorespiratory events.
Design/Methods: Single-center observational study including infants >1500g, < 44 weeks’ postmenstrual age (PMA), and off ventilator/CPAP support. A sample size of 70 subjects was estimated to provide sufficient power to demonstrate a sensitivity/specificity ≥80% with 90% paired agreement. Research staff and caregivers were masked to device output for the 48-hour study duration. We prospectively collected raw and processed data using a proprietary smoothing algorithm via portable Wi-Fi and standard hospital ECG electrodes and pulse oximetry (Nellcor, Mansfield, MA) from Philips MP70 monitors using Bedmaster (Anandic Medical Systems Inc., Feuerthalen, Switzerland). Data were time-aligned and analyzed using MATLAB to compare bradycardia and hypoxemia events. The co-primary outcome was the diagnostic accuracy of the Owlet OSS 3.0 for the detection of events with heart rate (HR) < 50bpm and oxygen saturations (SpO2) < 80% for ≥3 seconds. Secondary outcomes included pre-specified alternative bradycardia and hypoxemia thresholds.
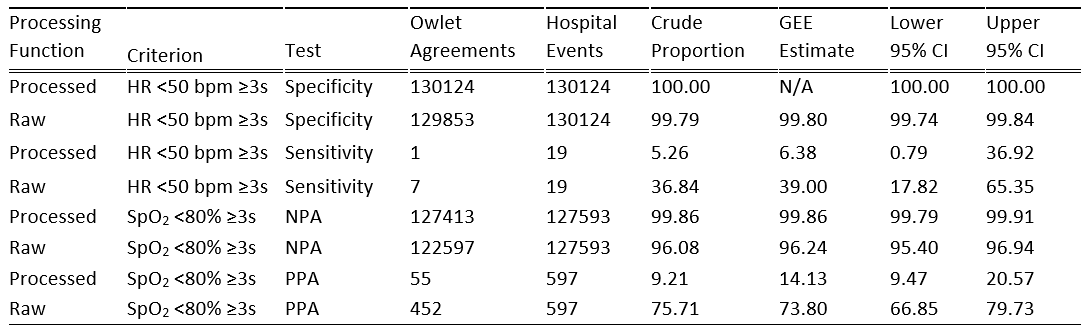
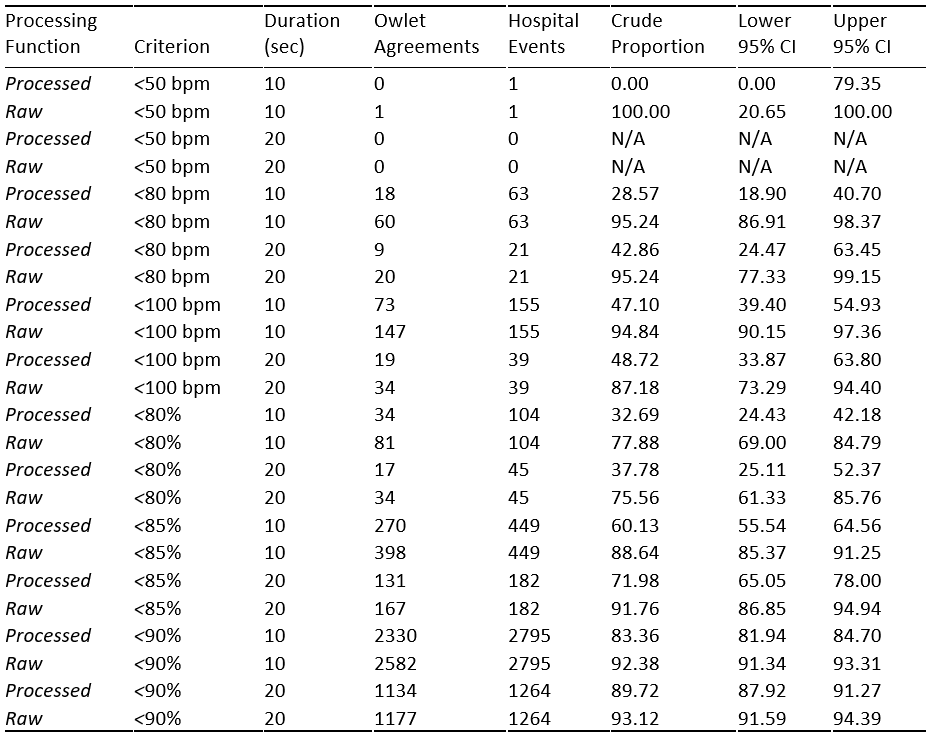
Results: We recorded data from 70 infants. The median gestational age was 31 weeks (range 23-40) and infants were studied at median 35 weeks’ PMA (range 32-42) weighing 1930g (range 1500-3605). The sensitivity for detection of HR < 50bpm ≥3s was 6% and 39% for processed and raw data, respectively, while the specificity was 100% and 100% for processed and raw data, respectively (Table 1). The positive percentage agreement for SpO2 < 80% ≥3s was 14% and 74% for processed and raw data, respectively, while the negative percentage agreement was 100% and 96% for processed and raw data, respectively. Detection of bradycardia and hypoxemia was higher for events with longer durations and/or when using higher thresholds (Table 2). In an exploratory analysis, device agreement for the 27 events with hospital monitor bradycardia or hypoxemia and a documented clinical intervention was 23/27 (85%) for processed and 26/27 (96%) for raw data.
Conclusion(s): The Owlet OSS 3.0 had 100% specificity for bradycardia < 50bpm and SpO2 < 80% events of ≥3s duration consistent with a low false alarm rate but did not meet predetermined sensitivity targets. Sensitivity was higher for raw data and for episodes of longer duration and for higher thresholds typically used in hospital settings.