Neonatology
Session: Neonatal General 6: POCUS, Technology in NICU
154 - Machine learning models accurately predict length of hospital stay for NOWS infants
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 154
Publication Number: 154.2264
Publication Number: 154.2264
Zachary A. Vesoulis, MD, MSCI
Assistant Professor
Washington University in St. Louis School of Medicine
St. Louis, Missouri, United States
Presenting Author(s)
Background: Neonatal Opioid Withdrawal Syndrome (NOWS) affects thousands of US infants each year. Optimal short-term outcomes are achieved through early discharge planning; however, the expected length of stay (LOS) is unknown early in the NICU course. Typical management includes serial examination and scoring of withdrawal symptoms using a subjective scale such as Finnegan Neonatal Absence Score (FNAS), yet these scores are used only for immediate management. Machine learning may identify patterns in FNAS data that predict prolonged LOS, and could support clinicians and families with discharge planning and expectations.
Objective: Use machine learning to identify patterns in early FNAS data that predict LOS greater than 14 days.
Design/Methods: A multicenter cohort of term infants with confirmed in utero exposure to opioids and admitting diagnosis of NOWS were retrospectively identified at 2 level IV NICUs. FNAS values and their timestamps were extracted from the medical record. Sex, gestational age, birth weight, and LOS in days were collected.
Our goal was to identify the most accurate prediction that could be made using the least amount of data, in order to provide the earliest and highest confidence guidance about need for extended hospitalization. Previous studies have reported a median LOS=14 days, thus we aimed to predict extended LOS (defined as >14 days) using FNAS values from early in the hospital course.
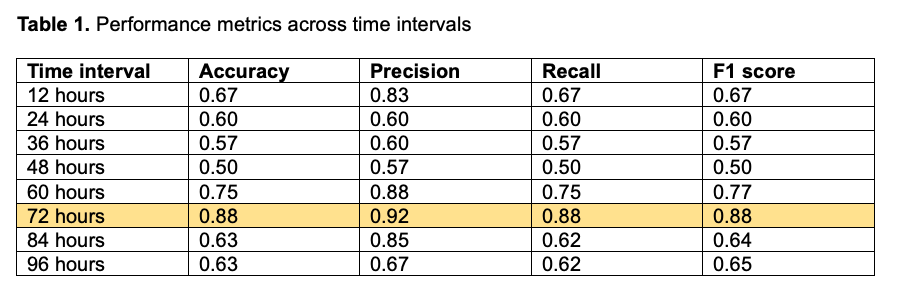
Infants were randomly divided into training and testing cohorts using a standard 80/20 split. We built a random forest classifier model with n_estimators=100 using the scikit-learn library for Python. We systematically evaluated model performance metrics using FNAS data intervals starting with 12 hours of data and increasing in 12-hour increments up to 96 hours. Performance was evaluated through precision, accuracy, recall, and F1 score.
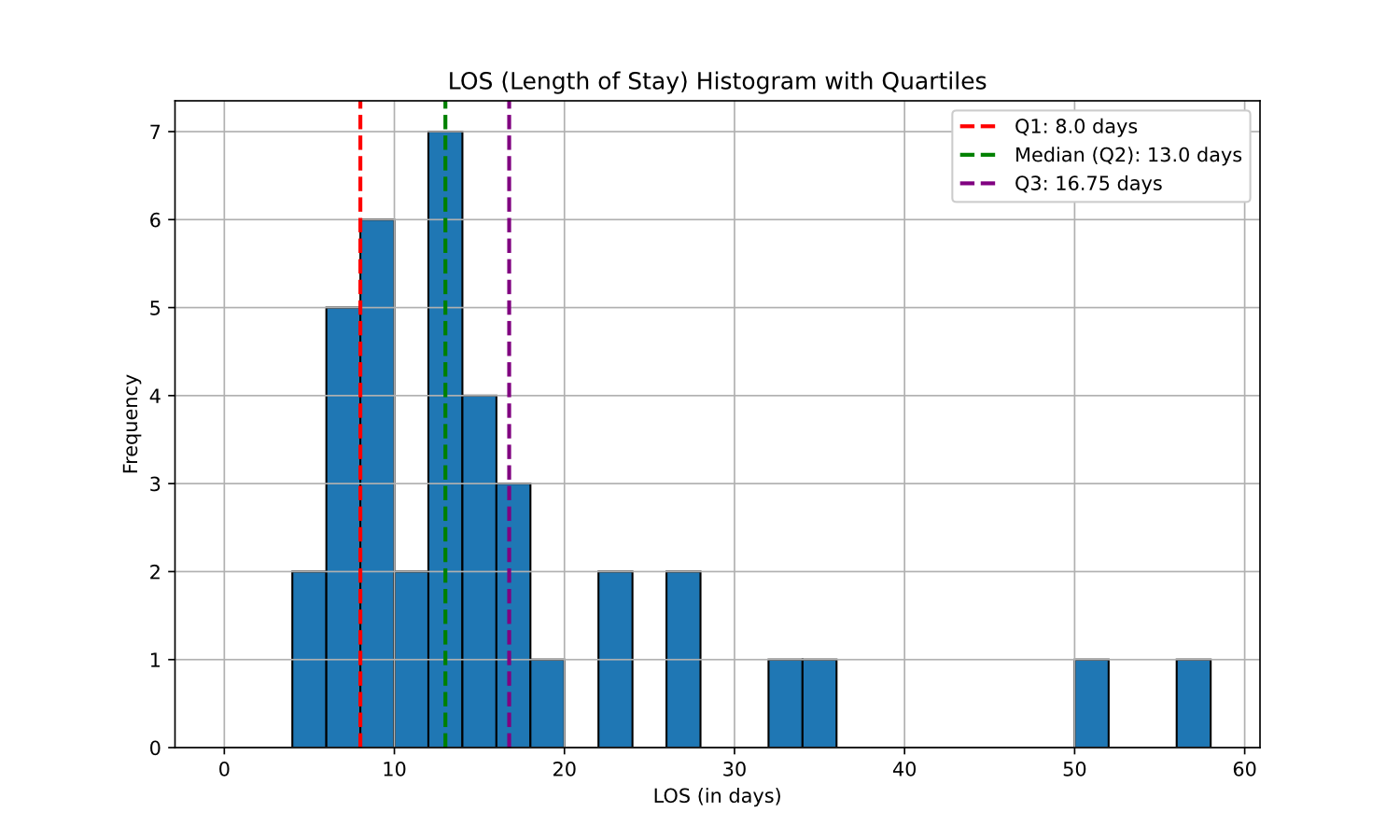
Results: We analyzed 43 infants with 2890 recorded FNAS values, who had mean GA=38.3 weeks, mean BW=2897g, and 35% were female. Median LOS was 13 days (20 infants >14d, 23 infants <=14 days; Figure 1). Infants with extended LOS had higher FNAS values in the first 4 days following birth (Figure 2). The machine learning model was able to predict LOS group across all time intervals, however a peak accuracy of 88% was achieved when using 72h of FNAS data (Table 1).
Conclusion(s): Using a machine learning model, FNAS data from the first 72 hours after birth predicted extended LOS (>14 days) with 88% accuracy in a multicenter cohort of term infants with NOWS. Additional study in a larger cohort and with polysubstance exposed infants may achieve greater accuracy.
.png)
