Neonatology
Session: Neonatal Neurology 8: Preclinical
324 - Neonatal Hypoxia-Ischemia Causes Aberrant Organization of the Brain Gliovascular Unit in Adult Humanized ApoE4 Mice
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 324
Publication Number: 324.2789
Publication Number: 324.2789
Raul Chavez-Valdez, MD (he/him/his)
Associate Professor
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
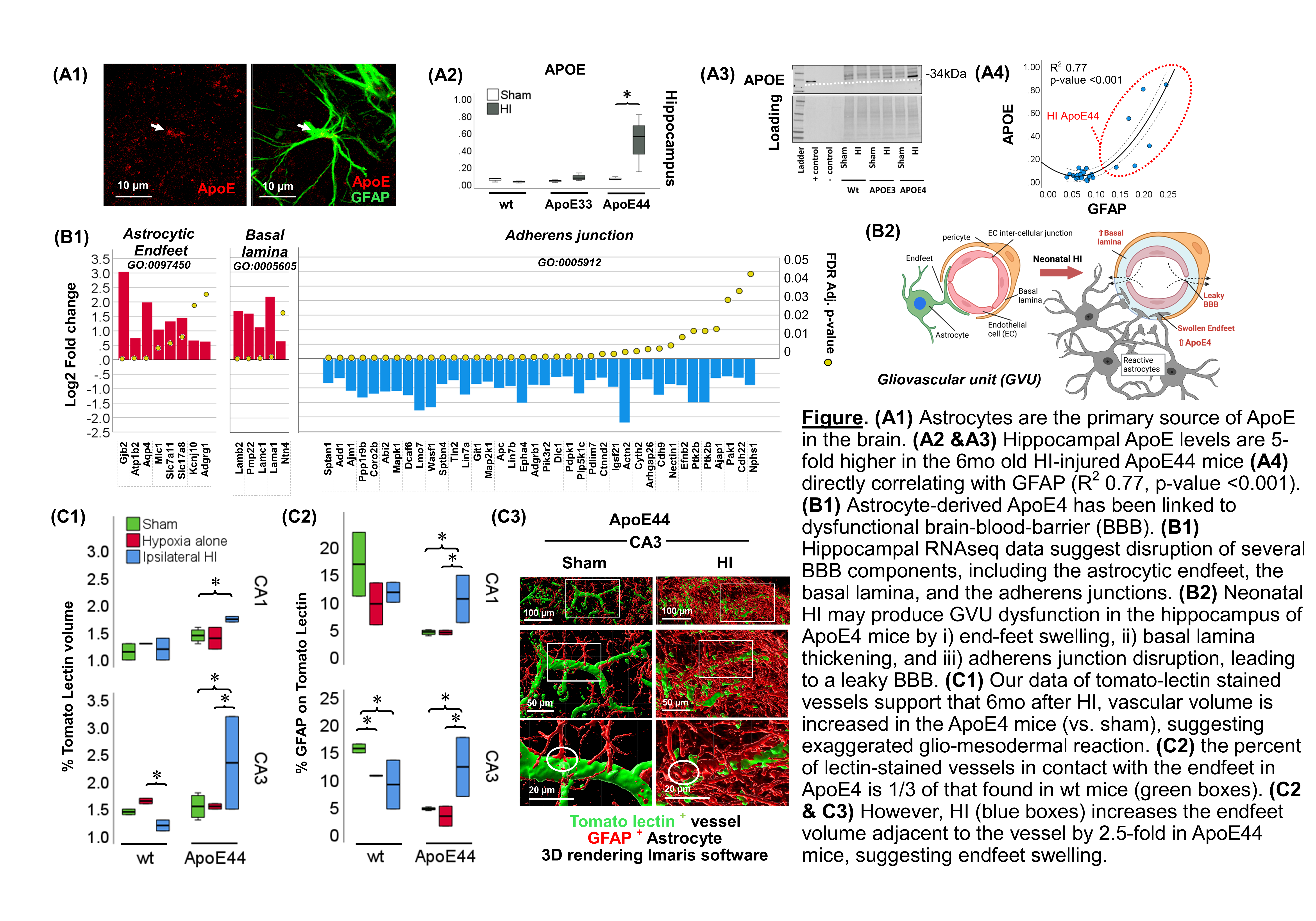
Background: Human ApoE4, a risk factor for some late neurodegeneration, is linked to smaller hippocampi (Hp) and impaired working memory in healthy children. Astrocytes, the primary source of brain ApoE4, are dysfunctional following neonatal hypoxia-ischemia (HI). Interactions between the astrocytic endfeet and vascular cells form the gliovascular unit (GVU), integral component of the brain blood barrier (BBB). Early GVU dysfunction follows neonatal HI, but the influence of ApoE4 in late GVU organization is unknown.
Objective: ApoE4 leads to dysfunctional BBB, thus we studied if 6 mo after HI ApoE4 would lead to late alterations in GVU with increased glio-mesodermal reaction (vascular overdevelopment), decreased endothelial junctional integrity and evidence of astrocytic endfeet swelling.
Design/Methods: HI brain injury (Vannucci) was produced on postnatal day (P)10 in ApoE humanized knock-in mice and compared to littermate shams and wildtype (wt) C57BL6 mice. Hp were studied at 6 mo for gene ontology (GO) RNAseq analysis and a combination of immunoblotting and IF-IHC with Imaris processing for GFAP, APOE, and tomato lectin-stained vessels.
Results: Astrocytes are a source of ApoE in the brain (A1). ApoE levels were 5-fold higher in the 6 mo HI-injured ApoE4 Hp (A2 & A3), directly correlating with GFAP levels (R2 = 0.77, p-value < 0.001, A4) suggesting response to ongoing astrocytic activation. RNAseq analysis suggested disruption of several Hp BBB components, including the astrocytic endfeet, the basal lamina, and the adherens junctions (B1) 6 mo after HI. Thus, HI may produce GVU dysfunction in the ApoE4 Hp by i) end-feet swelling, ii) basal lamina thickening, and iii) adherens junction disruption, leading to leaky Hp BBB 6 mo after HI (50 yo human equivalent) (B2). Imaris analysis showed increased vascular volume in Hp ApoE4 CA1 and CA3 (vs. sham), marking an exaggerated glio-mesodermal reaction (C1). The proportion of lectin-stained vessels in contact with GFAP+ endfeet in Hp ApoE4 was 1/3 of that found in wt (green boxes, C2). However, HI led to a 2.5-fold increase in endfeet volume adjacent to the vessel in the ApoE4 Hp, suggesting endfeet swelling.
Conclusion(s): As we have documented previously, ApoE4 leads to persistent reactivity and dysfunction of Hp astrocytes to adulthood after neonatal HI. This dysfunction comes along with an exaggerated glio-mesodermal reaction with evidence of astrocytic end-feet swelling and poor integrity of adherence junctions, pre-requisite for the assembly of BBB tight junctions. All together these data suggest a “leaky” Hp BBB through adulthood in HI-injured ApoE4 Hp.