Neonatology
Session: Neonatal Clinical Trials 1
470 - Multicenter Randomized Controlled Trial Comparing High Flow Nasal Cannula (HHHFNC) and Nasal Intermittent Positive Pressure Ventilation (NIPPV) Delivered by Long Narrow Tubing in Preterm Infants
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 470
Publication Number: 470.1125
Publication Number: 470.1125

Ayala Gover, MD (she/her/hers)
Medical Director Neonatal Intensive Care Unit
Bnai Zion Medical Center
Haifa, Hefa, Israel
Presenting Author(s)
Background: NIPPV provided by short nasal prongs was found to be more effective in preventing intubation compared to NCPAP as initial treatment of RDS and post extubation in preterm infants. Low narrow tubing (Ram cannula) which provides NIPPV (non-inferior to short prongs) has a softer and gentler interface, and causes less nasal trauma. HHHFNC has been found to be comparable to NCPAP in older preterm infants as primary treatment of RDS, or post extubation. However, there are no randomized controlled trials comparing the effectiveness of the two gentle interfaces; Ram-NIPPV and HHHFNC
Objective: To examine if HHHFNC is non-inferior to Ram-NIPPV when used as primary respiratory support or post extubation in preterm infants
Design/Methods: Multicenter prospective randomized controlled study, performed in 3 centers. Preterm infants born at 24-36+6 weeks of gestational age (GA) who were candidates for non-invasive respiratory support were randomized to HHHFNC (Vapotherm) or Ram-NIPPV. Infants ≤28 weeks GA were only eligible for recruitment after extubation. The primary outcome was treatment failure within 7 days defined as respiratory deterioration with increase in FiO2 (>50% or >30% change), respiratory acidosis (pH < 7.20 and PCO2>60), apneas (over 6 in 6 hrs) or need for emergency intubation. Infants failing HHHFNC were allowed to cross-over to Ram-NIPPV before intubation
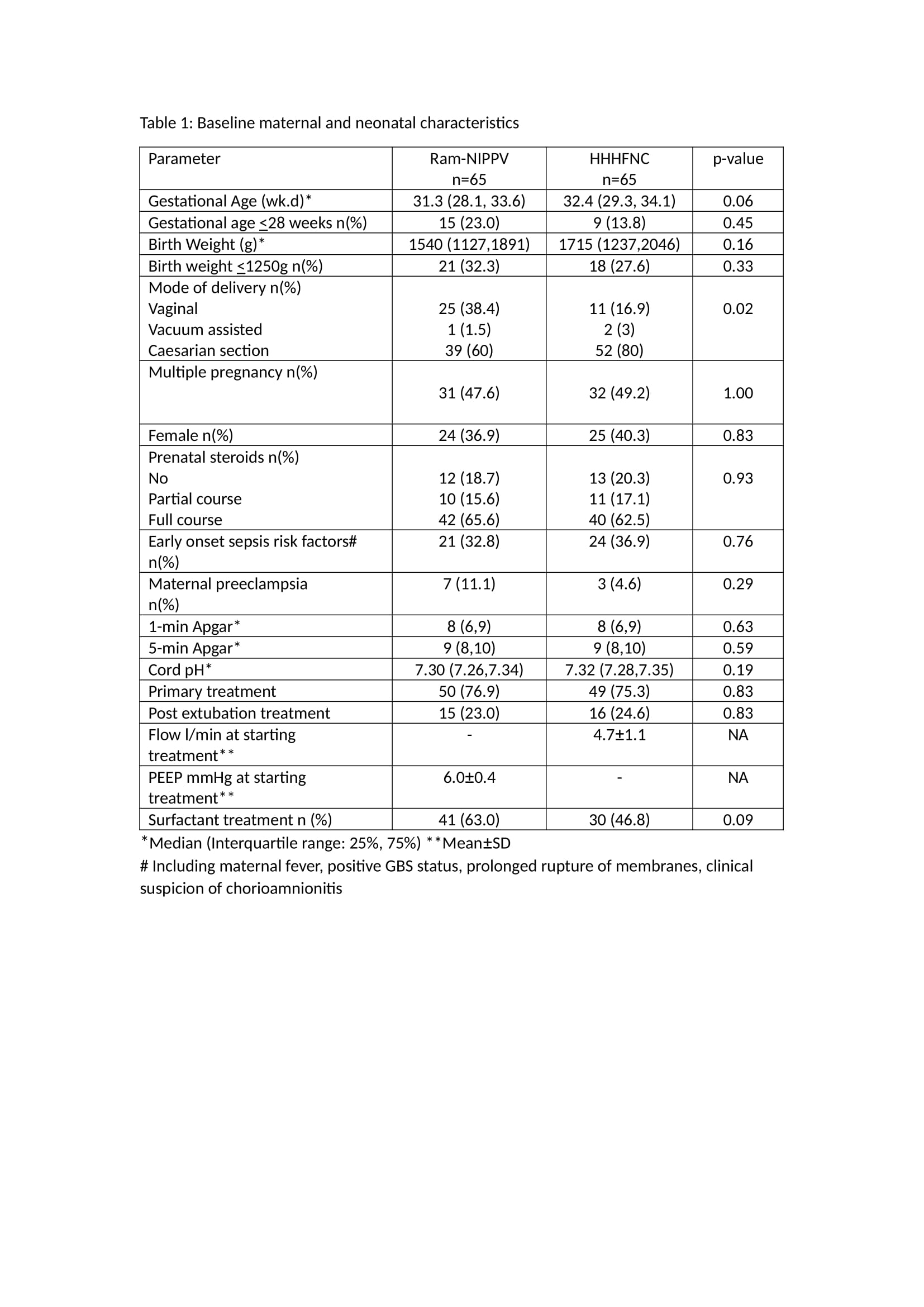
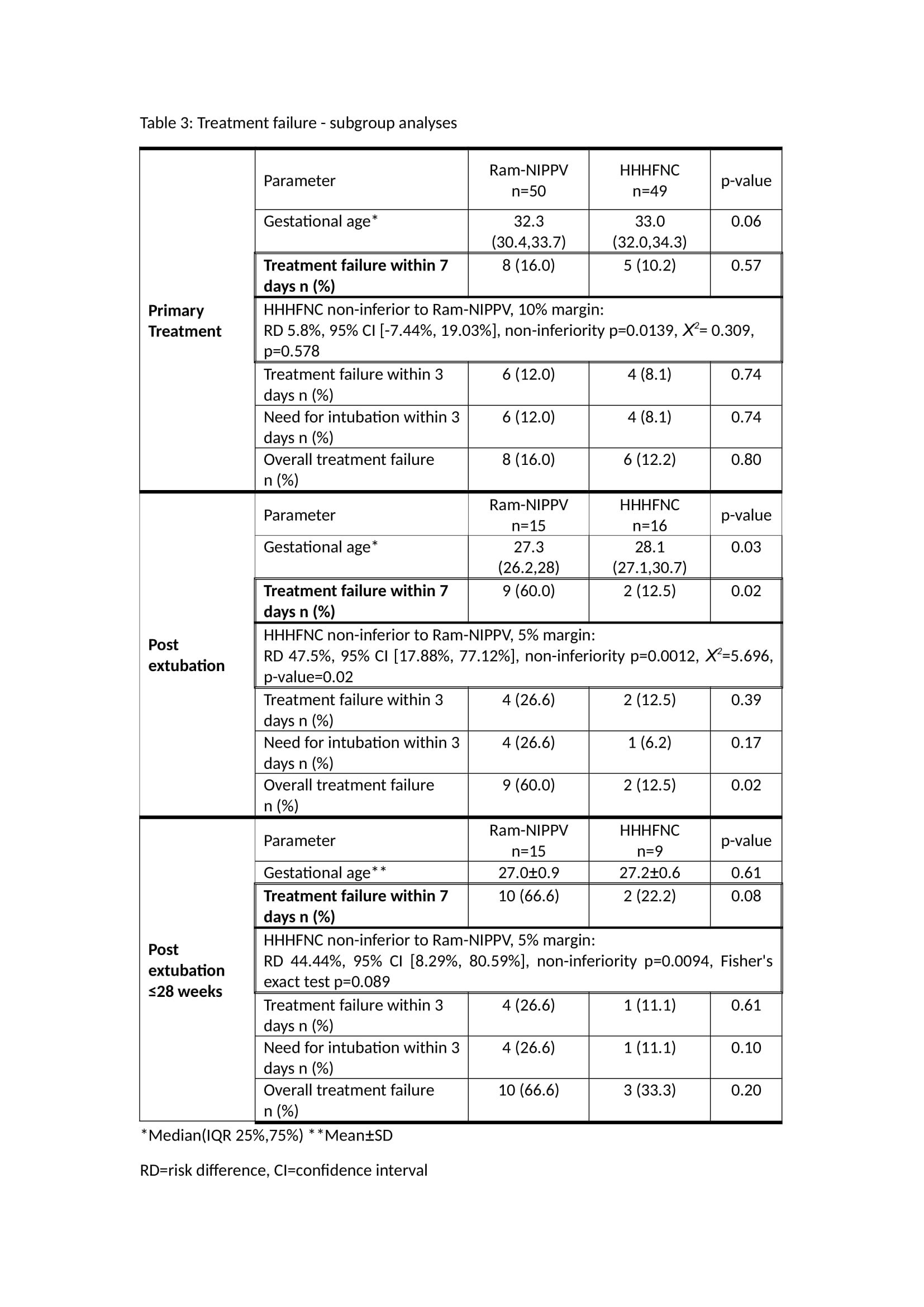
Results: The cohort comprised 130 infants: 65 infants in each arm. Baseline characteristics were comparable (Table 1), although gestational age and birth weight in the HHHFNC group were higher (NS). Most infants in the cohort were >28 weeks and >1250g, and most were recruited as primary treatment. HHHFNC was non-inferior to Ram-NIPPV (margin of 1.5%) in the primary outcome [risk difference (RD) 15.38%, 95% confidence interval (CI) [2.31%, 28.46%],non-inferiority p=0.0068, Χ2=4.139, p=0.042). Two out of 8 infants who failed HHHFNC were rescued by Ram-NIPPV and did not require intubation. In subgroup analyses, HHHFNC performed better than Ram-NIPPV as post-extubation respiratory support, however GA was significantly higher in this group (Table 3). HHHFNC was non-inferior to Ram-NIPPV in the primary outcome in infants >28 weeks receiving primary treatment (margin of 10%), and in infants ≤28 weeks treated post extubation (margin of 5%). HHHFNC was associated with less nasal trauma but with longer respiratory support.
Conclusion(s): In this study of mostly large preterm infants, HHHFNC was non-inferior to Ram-NIPPV in providing respiratory support to preterm infants, while causing less nasal trauma. Our findings cannot be generalized to infants ≤28 weeks