Neonatology
Session: Neonatal GI Physiology & NEC 3: GI Physiology and Probiotics
540 - Bloodstream Infections in Infants With Short Bowel Syndrome: An 11 Year Experience in a Tertiary Neonatal Intensive Care Unit
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 540
Publication Number: 540.2208
Publication Number: 540.2208

Muralidhar Premkumar, MBBS, MS (he/him/his)
Associate Professor
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Understanding the factors associated with bloodstream infections (BSI) in infants with short bowel syndrome (SBS) may help devise strategies to prevent BSI and decrease the associated mortality and morbidity.
Objective: To describe the profile of BSI and any associations with outcomes in infants with SBS in a single tertiary NICU.
Design/Methods: We included infants with SBS at Texas Children's Hospital (January 2011-June 2022). SBS was defined as a major intestinal resection ( < 50% of expected small bowel length or < 75 cm of small bowel remaining) followed by ≥ 90 days of parenteral nutrition (PN). BSI was defined by a positive blood culture (bacteria/ fungi) treated for ≥ 5 days. Fisher's exact test and logistic regression assessed the associations of BSI with mortality. Shapiro-Wilk test checked normality for secondary outcomes (hospital stay, TPN days). Normally and not normally distributed outcomes were compared using the t-test and Wilcoxon rank sum test, respectively.
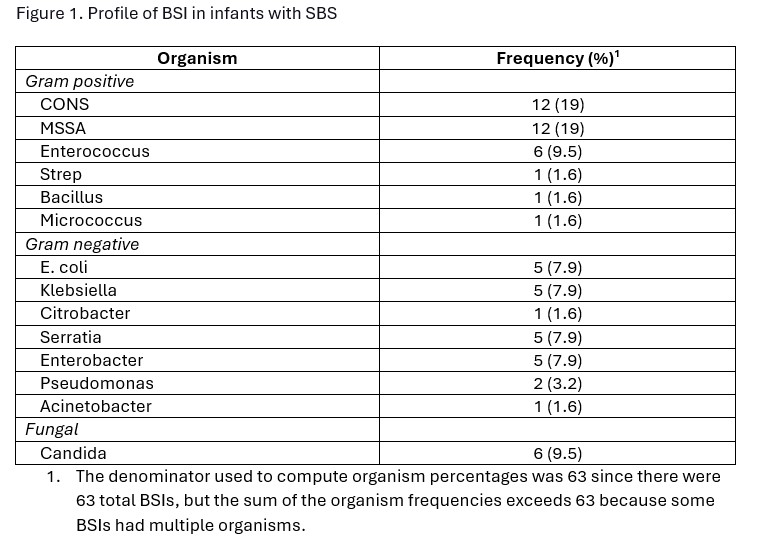
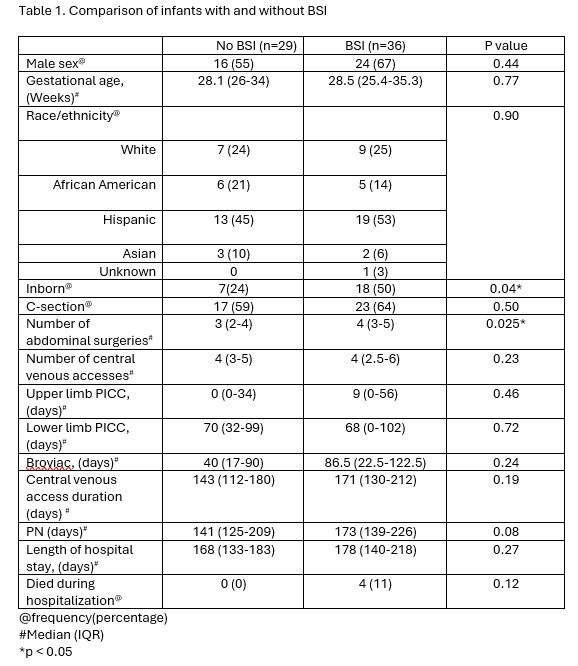
Results: 65 infants with an M: F ratio of 1.6 :1 had a median gestational age of 28.3 weeks (interquartile range (IQR): 25-34) and birth weight of 1.2 kg (IQR: 0.79-2.2). Necrotizing enterocolitis (59%) and gastroschisis (14%) were the common etiologies of SBS. The median duration of the PN requirement was 163 days (IQR: 131-215), and the median length of hospital stay was 170 days (IQR: 138-210). 36 (55%) infants had at least one BSI (total number of BSI = 63), and 18 (27%) infants had more than one episode of BSI. Gram-positive, gram-negative, and fungi caused 33 (52%), 24 (38%) and 6 (9%) of BSI respectively (Figure 1). 61 infants (94) survived until hospital discharge, with 36 (55%) infants achieved complete enteral autonomy, 25 (39%) were on PN. Four of 36 (11%) patients who had a BSI died during the initial hospitalization compared to 0/29 (0%) of those who did not have a BSI (p=0.122). Each BSI more than doubled the odds of death, but this association did not achieve statistical significance (odds ratio = 2.23, 95% confidence interval: 0.93 – 5.34, p = 0.073). Patients with at least one BSI had significantly more abdominal surgeries (p = 0.025) and trended towards longer PN days (median 141 vs. 173; p = 0.08) (Table 1).
Conclusion(s): Infants with SBS are at a high risk for BSI. The association of the number of abdominal surgeries with BSI and the trend towards longer PN duration in BSI patients highlights the complexities of SBS in those infants. This data and the knowledge gained regarding BSI in infants with SBS will help us understand the risk factors, prognosticate, and devise strategies to improve outcomes.