Neonatology
Session: Neonatal Pulmonology - Clinical Science 6: Respiratory/Neuro Outcomes, Steroids
587 - Can we predict Outcomes for Premature Infants Referred to a Quarternary NICU for Respiratory Escalation?
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 587
Publication Number: 587.2980
Publication Number: 587.2980
- ds
dafne A. sanabria Garcia, fellow (she/her/hers)
PGY-6
Children's Hospital of Michigan
detroit, Michigan, United States
Presenting Author(s)
Background: Severe bronchopulmonary dysplasia is associated with risks of death and need for long-term ventilation via tracheostomy. Preterm infants who persistently require respiratory support as they approach 36 weeks postmenstrual age (PMA) are evaluated, although variably, for tracheostomy; this often involves transfer to a higher level Neonatal Intensive Care Unit (NICU). Data to guide whether, when and which infants would need escalation of care and their associated outcomes are limited.
Objective: To describe short-term outcomes and evaluate risk factors predictive of death or tracheostomy (D/T) among high-risk preterm neonates on respiratory support referred to a regional NICU for respiratory indications at ≥34 weeks PMA .
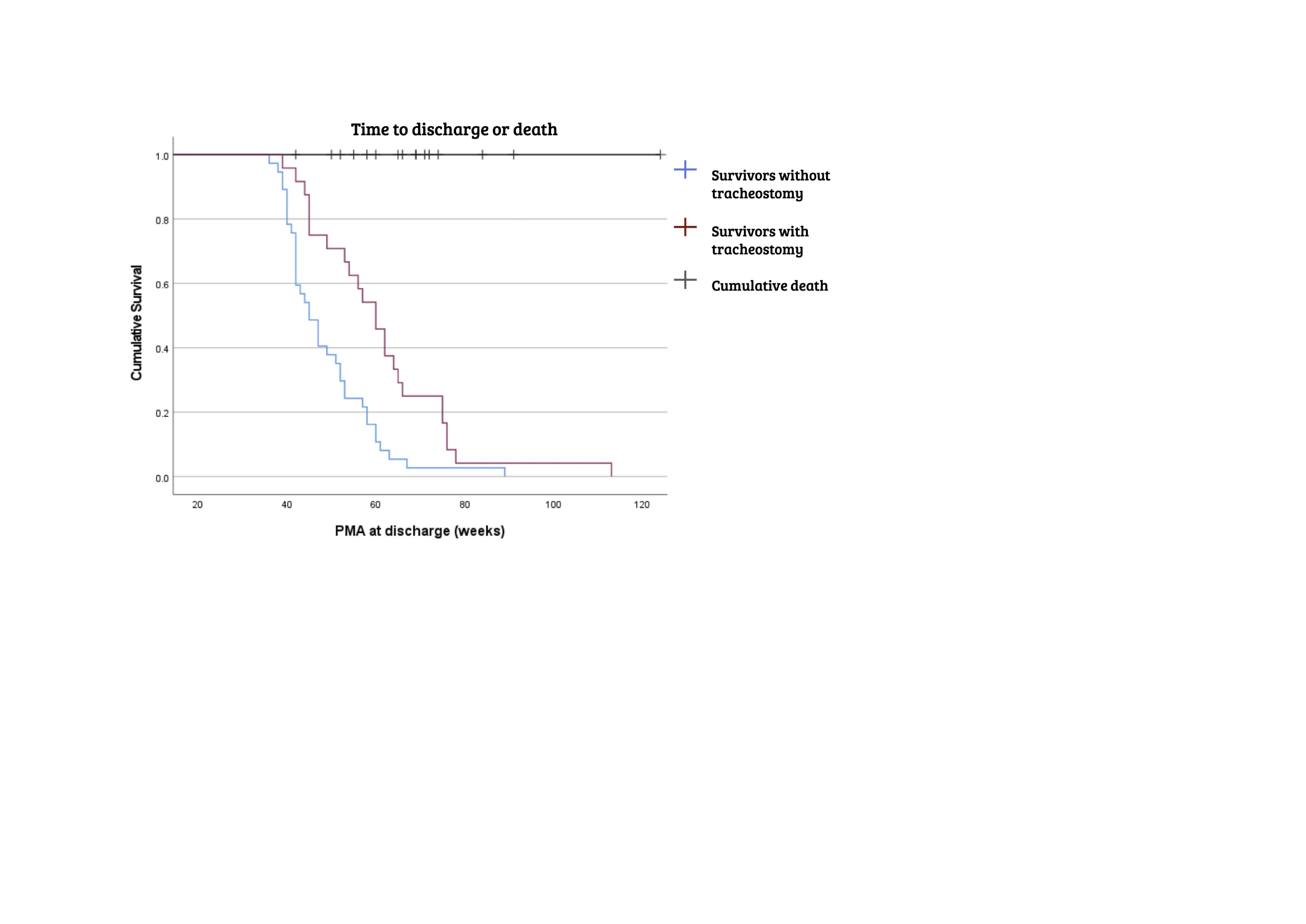
Design/Methods: This single center retrospective review included preterm neonates (gestational age-GA < 30 weeks) who were on respiratory support (mechanical ventilation, CPAP, high flow canula ≥2 liters or FiO2 > 30%) referred from level III NICUs for respiratory indications at ≥34 weeks PMA over a 10-year period (2013-2022). Infants who were transferred out were excluded. Medical records were reviewed to abstract birth and pre-admission data as well as respiratory support (FiO2, respiratory severity score) at admission, and specific timepoints (36-, 40- and 44-weeks PMA and 1 week after admission). Statistical analysis included chi-square and t-test and binary logistic regression. Kaplan Meir curves were used to compare length of NICU stay in groups.
Results: The cohort (n=77) was predominantly [43 (55%)] male, [49 (63%)] black and [56 (72%)] born via C-section; mean (SD) GA was 25.4 (1.6) weeks and birth weight was 706 (177) grams. Death occurred in 16 (21%) infants, 3 without tracheostomy. There were significant differences between D/T [40 (52%)] vs. survivors without a tracheostomy [37 (48%)] groups in maternal hypertension, delivery mode, and infant sex. The admission PMA and respiratory support level were higher in the D/T group [Table1]. On logistic regression, higher admission respiratory support and PMA were significantly predictive of D/T but admission nitric oxide and FiO2, respiratory distress syndrome and sex were not [Table 2]. Figure 1 shows significant differences in length of NICU stay between groups.
Conclusion(s): About half of the preterm neonates who were referred to a quarternary NICU at ≥ 34 weeks PMA for respiratory escalation died or underwent tracheostomy; later PMA and higher respiratory support at admission were predictors of this adverse outcome. These data provide novel insights for clinicians and families to facilitate decision-making on tracheostomy.
.jpg)
.jpg)