Neonatology
Session: Neonatal Neurology 1: Clinical
8 - Effects of Caffeine on Infants with Hypoxic Ischemic Encephalopathy Undergoing Therapeutic Hypothermia
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 8
Publication Number: 8.417
Publication Number: 8.417
- RL
Rakesh Lavu, MD (he/him/his)
Fellow
Cleveland Clinic Children's
beachwood, Ohio, United States
Presenting Author(s)
Background: Therapeutic hypothermia is currently the standard of care for infants with moderate to severe Hypoxic Ischemic Encephalopathy (HIE). Several adjuvant therapies have been used to improve the neurodevelopmental outcomes in these infants. Caffeine, in addition to its diuretic effect on the kidney, has shown potential neuroprotective benefit in animal studies. The effects of caffeine on infants with HIE undergoing therapeutic hypothermia are still unknown.
Objective: 1.To compare the changes in urine output and renal function in infants who did and did not receive caffeine while undergoing therapeutic hypothermia for moderate to severe HIE.
2. To compare the short-term outcomes such as Seizures, MRI findings, EEG changes, length of stay and mortality during NICU stay in both groups.
Design/Methods: This is a retrospective cohort study from January 2013 – December 2022. We reviewed charts of neonates born ≥35 weeks of GA, who were admitted with a diagnosis of moderate to severe HIE and treated with therapeutic hypothermia. Infants with severe congenital malformations or chromosomal anomalies were excluded from the study. The caffeine group received a one time 20 mg/kg dose of caffeine.
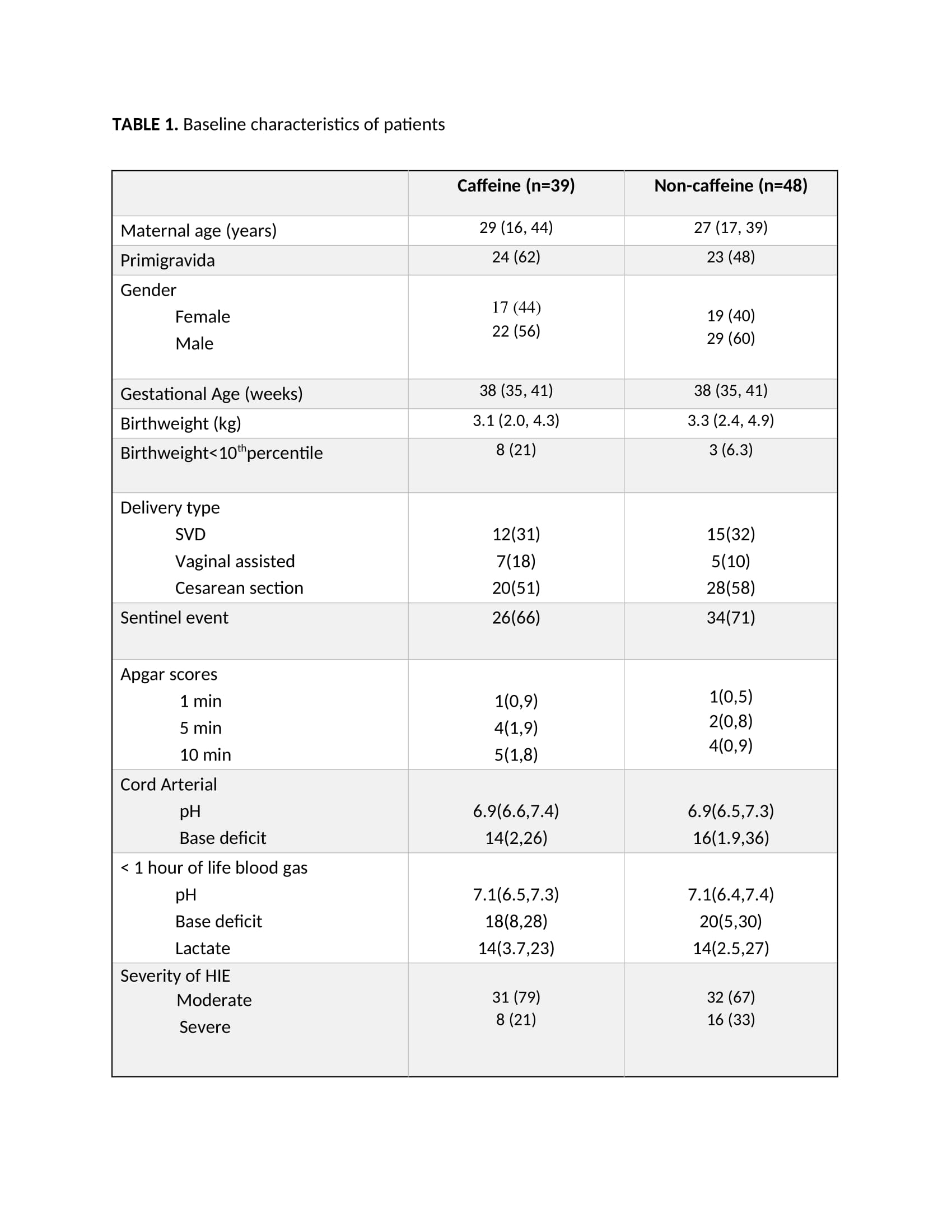
Results: A total of 87 infants underwent therapeutic hypothermia for moderate to severe HIE, of which 39 infants (45%) received caffeine with median time of administration being at 6 hours of life. Both the groups had similar baseline characteristics.
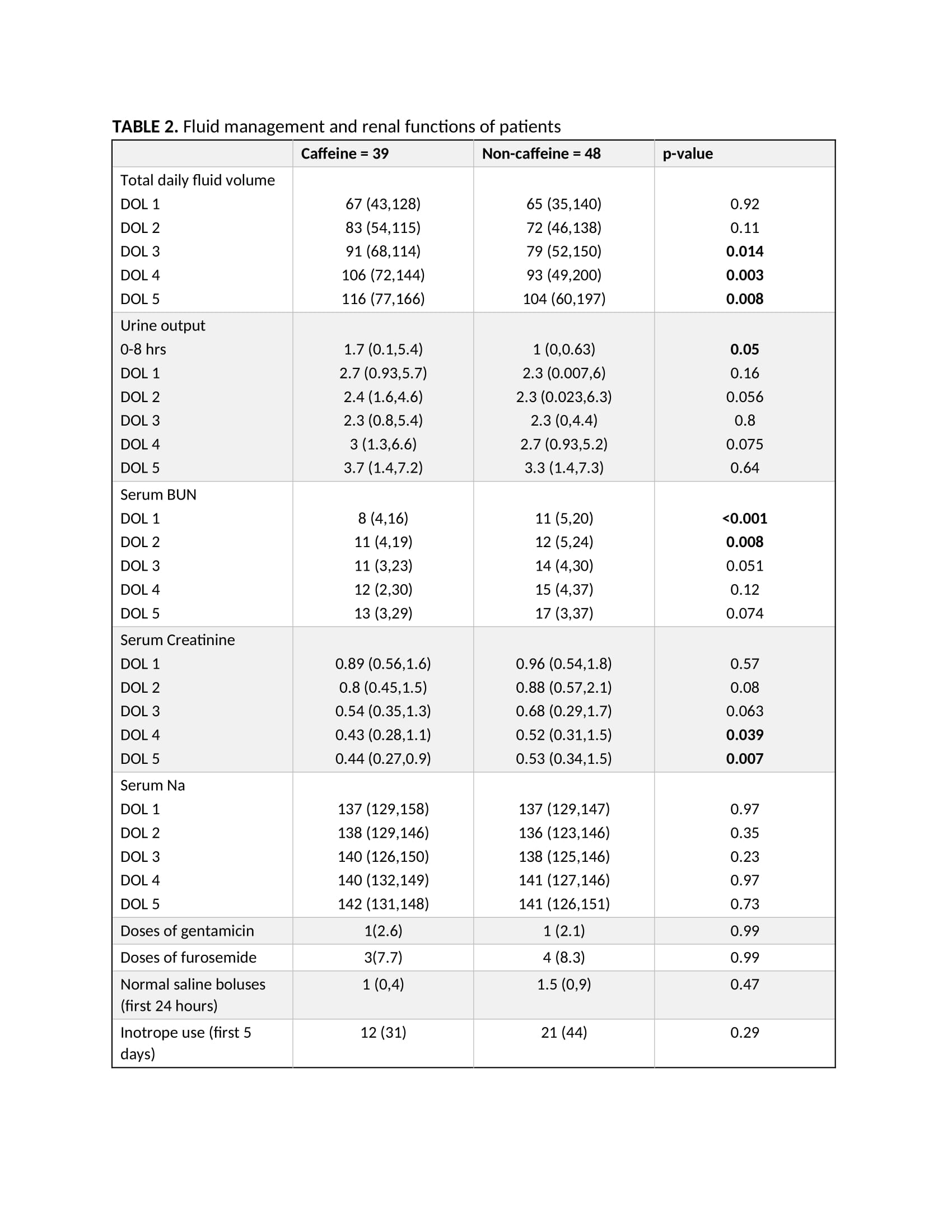
There was overall improvement in the urine output in infants who received caffeine, particularly in the first 8 hrs of life with median urine output of 1.7 vs 1 cc/kg/hr. Caffeine receiving neonates had better renal function with significantly lower BUN levels in first two days of life (8,11 vs 11,12) and lower serum creatine levels on DOL 4 (0.43 vs 0.52) and DOL 5 (0.44 vs 0.53).
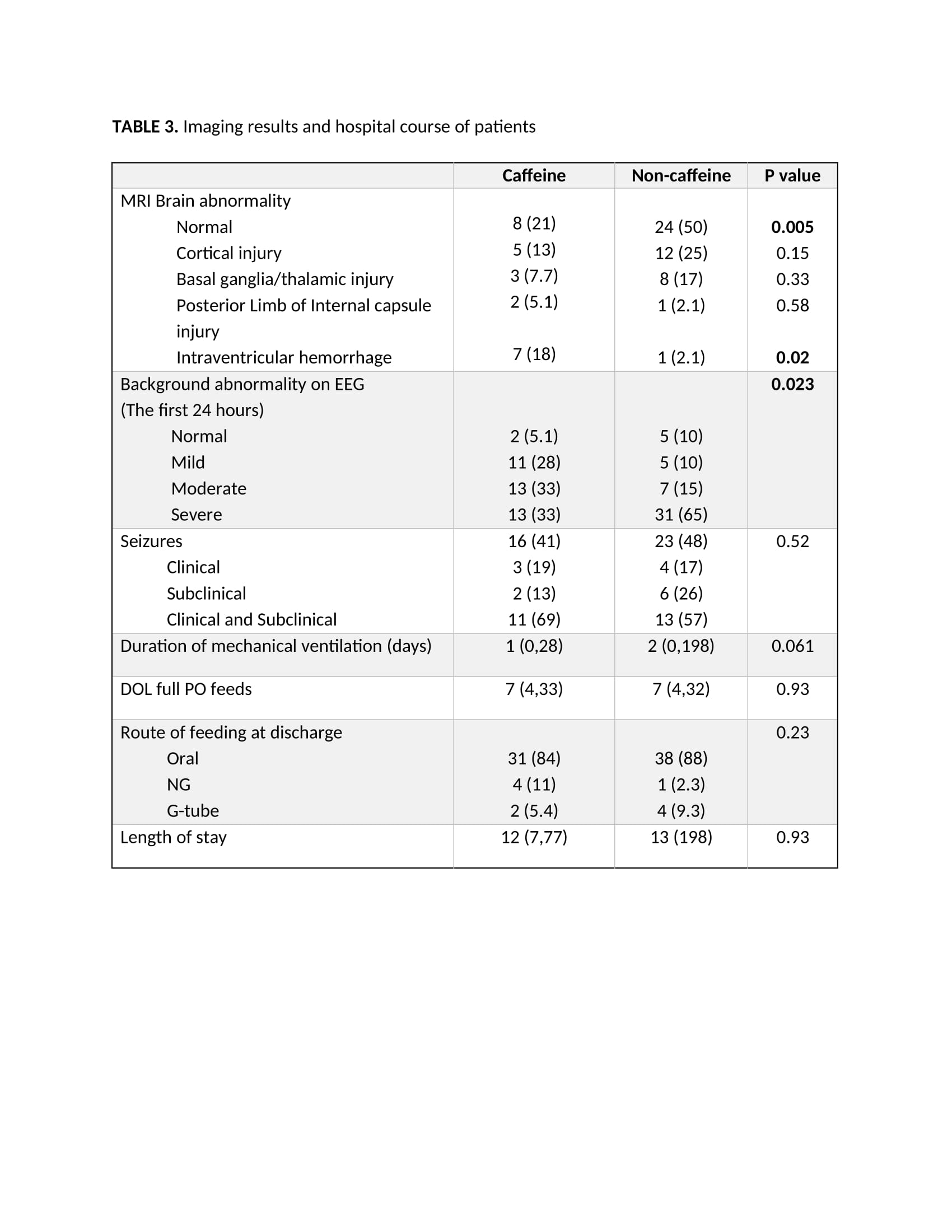
Infants who received caffeine had a significantly smaller proportion with normal MRI findings (21% vs 50%, p= 0.005) and had an increased incidence of IVH (18% vs 2.1%, p=0.02) when compared to non-caffeine group. Non-caffeine group had higher level of background EEG abnormality in the first 24 hours of life compared to caffeine group (p=0.023), however there was no difference in seizure frequency, length of stay or mortality between the groups.
Conclusion(s): The use of caffeine in neonates with HIE undergoing hypothermia was associated with an improvement in UOP and renal function. However, it was associated with a higher proportion of infants with abnormal MRI findings. A randomized trial will be needed to establish the efficacy and safety of caffeine in infants with HIE.