Neonatology
Session: Neonatal Pulmonology - Clinical Science 1: BPD, BPD Biomarkers and Diagnosis
188 - Airway colonization alters the tracheo-alveolar inflammatory profile in mechanically ventilated extremely preterm infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 188
Publication Number: 188.3055
Publication Number: 188.3055
- VC
Veronica Caballero, MD
Fellow
Holtz Children's Hospital Jackson Memorial Hospital
Miami Springs, Florida, United States
Presenting Author(s)
Background: The respiratory tract of extreme preterm mechanically ventilated infants is often colonized with bacteria. Inflammation contributes to lung disease, but it is unclear if pathogenic colonization elicits inflammation and if there are differential effects related to the type of colonizing organism.
Objective: To evaluate differences in the inflammatory profile of tracheo-alveolar fluid (TAF) of mechanically ventilated preterm infants before and after the first respiratory colonization with gram positive (GP) and gram negative (GN) bacteria.
Design/Methods: TAF was collected weekly during the first 4 w from intubated infants of 23-28 w gestation. Routine weekly TAF cultures were analyzed in microbiology laboratory. TAF inflammatory markers were measured by multiplex assay and normalized to protein concentration. For analysis, infants were selected when a TAF was collected within 5 days before and after the first colonization. Inflammatory markers pre- and post- first colonization were compared between groups colonized with GP or GN, or both.
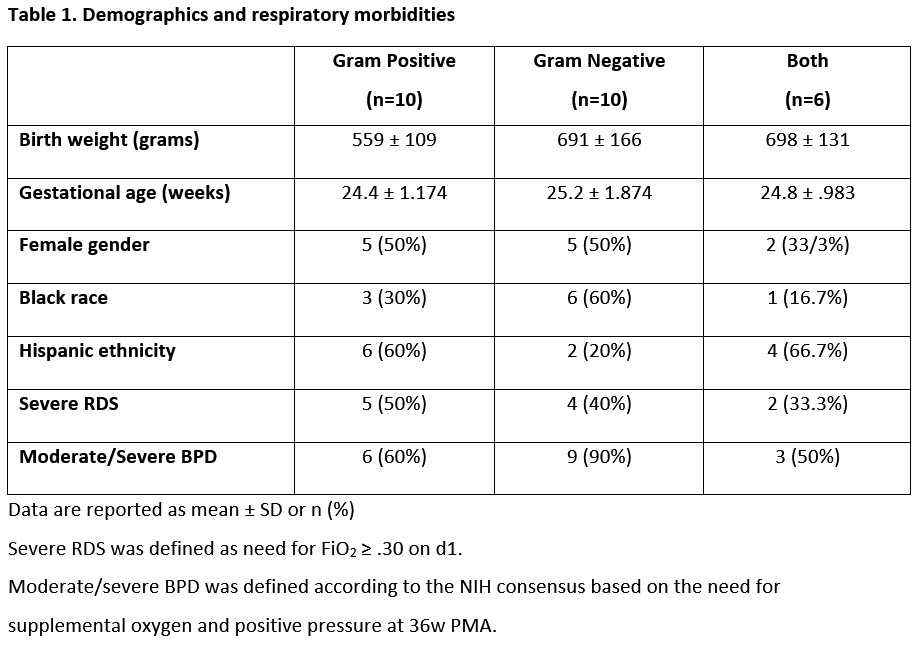
Results: 90 infants were enrolled. Of these, 26 mechanically ventilated infants were selected based on availability of TAF samples pre- and post- first colonization. 10 infants were colonized with GP and 10 with GN. Six infants were colonized with both. There were no differences between those colonized with GP, GN or both in regards to demographics and severity of RDS (Table 1).
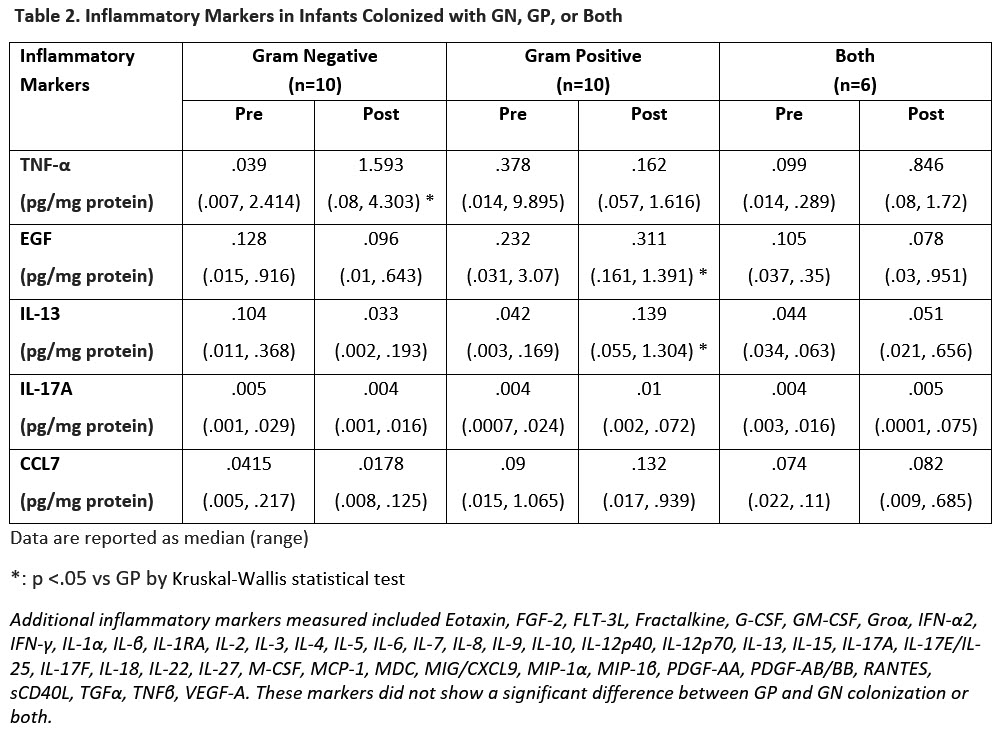
Inflammatory markers in pre-colonization TAF did not differ between infants colonized with GN, GP bacteria, or both (Table 2). In post-colonization TAF, tumor necrosis factor-α (TNF-α) was higher in GN compared to GP colonized infants. Epidermal growth factor (EGF), Interleukin-13 (IL-13) and Chemokine C-C motif ligand 7 (CCL7 aka MCP-3) were higher in GP compared to GN colonized infants. Colonization with both bacteria did not differ compared to colonization with GP or GN only.
Nine out of 10 infants colonized with GN eventually were classified as moderate to severe BPD at 36 w PMA compared to 6 out of 10 infants colonized with GP.
Conclusion(s): TNFα was higher in GN colonized while CCL-7, EGF, and IL-13 were lower compared to GP. Higher TNFα levels indicate a higher proinflammatory state in GN colonized. Higher CCL-7, EGF, and IL-13 levels indicate an anti-inflammatory state and enhanced immune response in GP compared to GN colonization. This is a possible mechanism for a worse respiratory evolution in infants colonized with GN. Replication of these findings in a large cohort may help development of preventive or therapeutic strategies. Supported by NHLBI grants (U01 HL133689, UO1 HL133708).