Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 5
38 - Reducing Central Line Bloodstream Infections (CLABSIs) at a Level 4 Regional Neonatal Intensive Care Unit (NICU)
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 38
Publication Number: 38.3018
Publication Number: 38.3018

Anna Ford (she/her/hers)
Medical Student
University of Illinois College of Medicine
Lemont, Illinois, United States
Presenting Author(s)
Background: Premature neonates are at high risk of infection due to immature skin barriers and immune
systems. These patients often require a high level of care supported by central lines.
Placement, monitoring, and maintaining the environment of each central line is crucial to
preventing life-threatening infections in the NICU.
Objective: Our SMART AIM is to decrease CLABSI rates in the NICU from 2.07 per 1000 days to 1.5 per
1000 days by July 2024.
Design/Methods: We engaged a multidisciplinary team involving neonatologists, APNs, NICU nurses, infection
prevention specialists, and administrators in the Fall of 2022 who met monthly to discuss
interventions for CLABSI prevention.
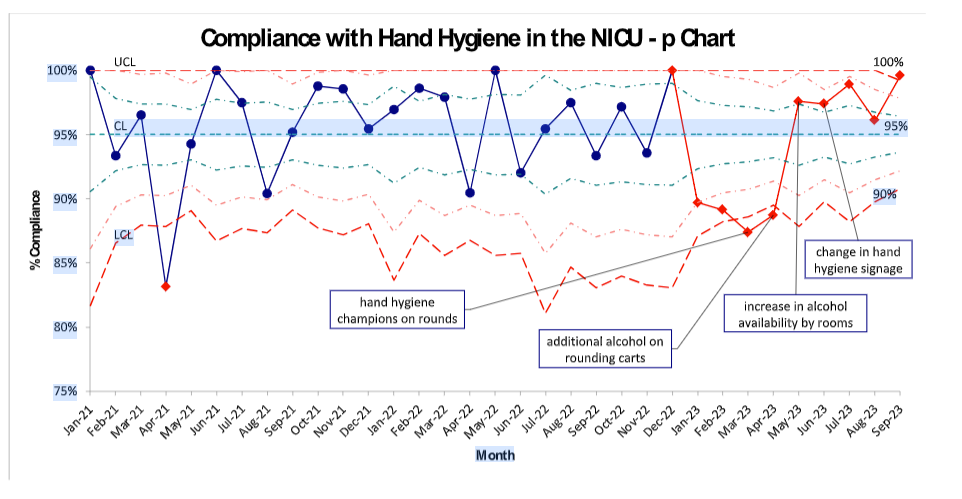
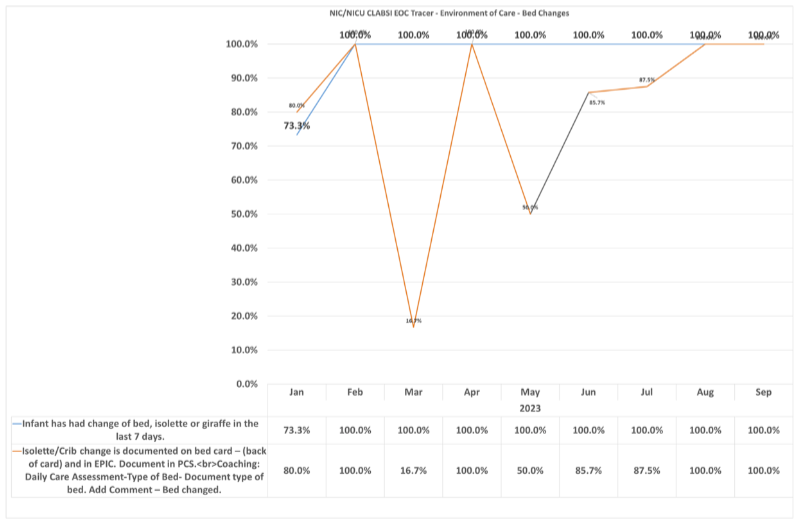
Major interventions included: 1. Improving compliance with hand hygiene. 2. Improving
cleanliness of the patient environment. 3. Initiation of UV sterilization. 4. Creation of a formal
CLABSI bundle. 5. Institution of sterile tubing changes. 6. Optimizing documentation for cases
of secondary bacteremia. Multiple PDSA cycles were performed for each major intervention.
The main outcome measure was the rate of CLABSIs per 1000-line days as well as days
between CLABSIs on the unit. Process measures included hand washing audits and
environmental care tracer audits from the infection and prevention team. Balancing measures
have included staff satisfaction.
Results: The monthly CLABSI rate has remained stable throughout the time period. However, our unit was
able to go 153 days without a CLABSI in 2023, demonstrating progress. Compliance with hand hygiene has improved
over the last 5 months to 95% through effective interventions. Focused nursing education and
audits to improve the cleanliness of the patient environment have improved over time.
Conclusion(s): A combination of the implemented strategies led to a 153 day CLABSI-free period along with an
improvement in hand hygiene compliance in the unit and an increase in engagement of NICU
staff in CLABSI prevention. Through the utilization of PDSA cycles the team has identified further
areas of opportunity including the use of non-sterile gloves during care for patients with central
lines and alternative products to decrease direct access of lines by nursing staff.
.png)