Neonatology
Session: Neonatal/Infant Resuscitation 3
293 - Surgical Delivery Risk Stratification in the Setting of Prenatally Identified Fetal Anomalies
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 293
Publication Number: 293.3279
Publication Number: 293.3279

Mekala Neelakantan, MD (she/her/hers)
Resident Physician
University of Michigan Medical School
Canton, Michigan, United States
Presenting Author(s)
Background: Neonates with prenatally diagnosed fetal anomalies require careful planning for stabilization and evaluation postnatally. The benefit of a timed delivery in the operating room, resuscitation by the neonatology team, and expeditious evaluation by subspecialists must be balanced with the consequence of separating the mother-infant dyad. To facilitate multidisciplinary care for neonates with the goal of maximizing safe bonding, a delivery risk stratification tool “MINT” (Michigan Initial Neonatal Treatment) was designed and implemented.
Objective: The aim of this study was to evaluate the safety and efficacy of the MINT risk delivery stratification tool for prenatally diagnosed surgical anomalies.
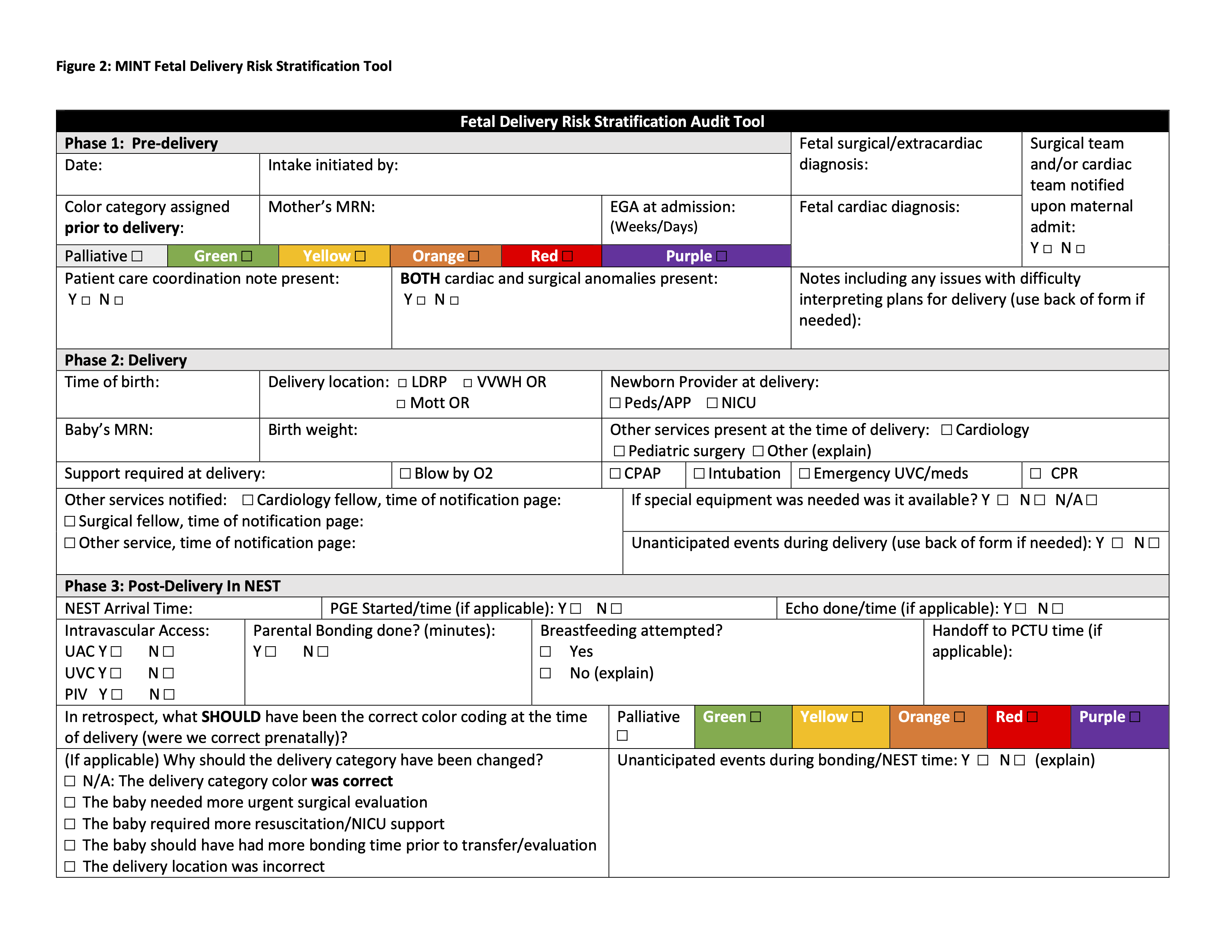
Design/Methods: A risk stratification system for infants with fetal surgical anomalies was designed, mirroring a previously established color-coded algorithm used to categorize infants with congenital cardiac disease at our center. The MINT system evaluates 3 phases surrounding a neonate’s birth (Pre-Delivery; Delivery; and Post-Delivery). Infants were assigned a color-coded risk stratification based on diagnosis (Figure 1) indicating location of delivery, which members of the multidisciplinary team must be present, and whether it was permissible for the infant to bond with parents prior to postnatal evaluation. All deliveries assigned a color-coded risk category were audited using a tool (Figure 2) to determine safety, accuracy of risk stratification assignment, and compliance with parent/infant bonding time. Weighted Kappa and Fisher’s exact analyses were used to compare audit data for infants classified using the surgical MINT system.
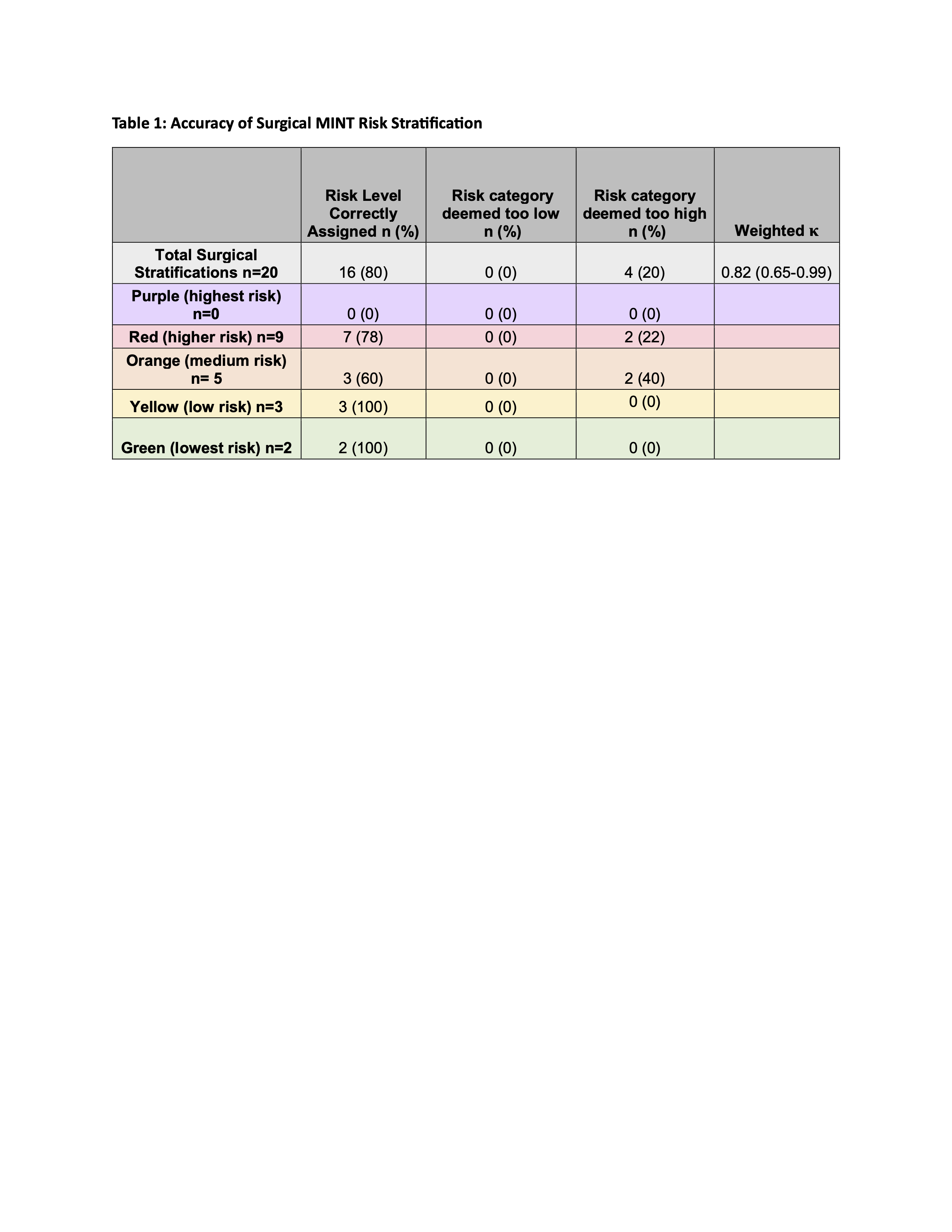
Results: 50 patients were assigned a MINT risk stratification between 03/23 and 08/23, 42 had completed delivery audits. 20 (47%) of patients had primary surgical diagnosis and 22 (53%) had primary cardiac diagnosis (comparison group). In the surgical group, 16 patients (80%) were correctly categorized prenatally with a weighted kappa of 0.82 (0.65-0.99). The accuracy was not statistically significant between cardiac and surgical groups (p= 0.72), demonstrating prenatal risk assignments were well correlated in both groups. No patients assigned an incorrect risk category in the surgical group required escalation of care (all were classified at a higher risk category than needed (Table 1)). No serious adverse events were reported.
Conclusion(s): Standardized risk stratification for neonates with fetal anomalies can be safely implemented to promote efficient utilization of personnel, equipment, and preserve parent/infant bonding.