Neonatology
Session: Neonatal-Perinatal Health Care Delivery: Practices and Procedures 1
444 - Multi-angle Video Assessment of Simulated Neonatal Intubation
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 444
Publication Number: 444.3220
Publication Number: 444.3220

Hannah S. Gu, MD (she/her/hers)
Neonatology Fellow
Lucile Packard Children's Hospital Stanford
Palo Alto, California, United States
Presenting Author(s)
Background: Neonatal intubation is a life-saving intervention with few objective markers of proficiency. Quantifying differences in novice and expert intubation technique is necessary to optimize training. Limited video data exists exploring the technical aspects of neonatal intubation, particularly in preterm neonates, even in simulation.
Objective: To use multi-angle video technology to quantify differences in intubation technique between novice and expert intubators in simulation.
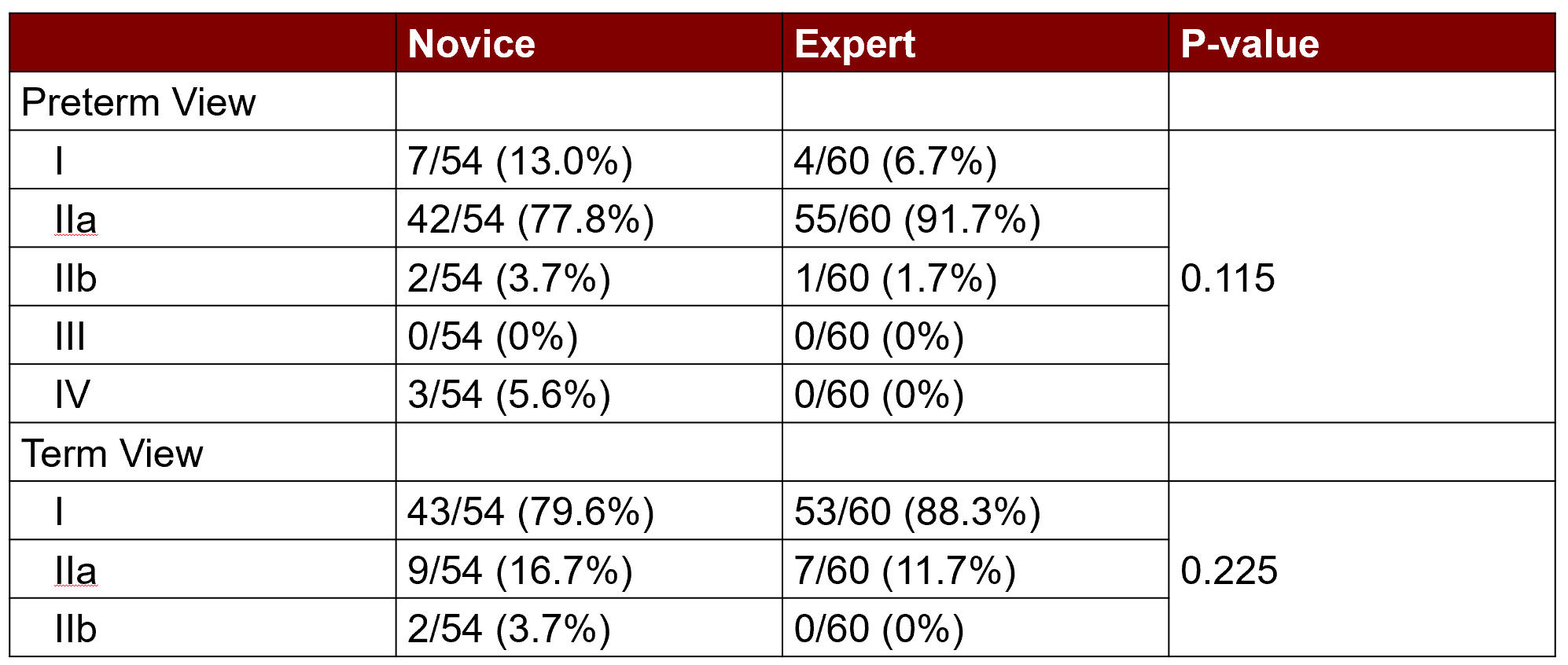
Design/Methods: Study subjects included attending neonatologists, neonatal hospitalists, neonatology fellows, pediatric residents, neonatal nurse practitioners, and registered nurse transport specialists. Experts were defined as: >10 intubations and >1 yr experience in the NICU. All others were novices. Each subject performed three intubation attempts using a video laryngoscope on both term and preterm neonatal manikins. Subjects were blinded to the video view. Intubation success was determined by intraoral visualization of endotracheal tube (ETT) passage through the vocal cords and auscultation. Overhead and intraoral video were used. We divided the intubation procedure into temporal epochs and recorded the best Cormack-Lehane view grade obtained (Figure 1). Statistical analyses included Mann-Whitney U tests and Fischer Exact tests.
Results: 38 study subjects were recruited. 20 were experts, and 18 were novices. 228 intubation trials were analyzed, 12 of which were unsuccessful (4 expert, 8 novice). The median time to intubate the preterm manikin for experts was 15.7 sec compared to 17.9 sec for novices (p=0.121). The median time to intubate the term manikin for an expert was 12.5 sec compared to 15.8 sec for a novice (p < 0.001). In the preterm manikin, the longest epoch for both novices and experts was viewing the cords after the blade enters the mouth; experts completed this significantly faster than novices. In the term manikin, the most time-consuming epoch for both novices and experts was manipulating the ETT into intraoral view after recognizing a view of the cords; experts also completed this significantly faster than novices (Figure 2). There were no significant differences in Cormack-Lehane view grade obtained by novices and experts in either the term or preterm manikin (Table 1).
Conclusion(s): Based on experiential and dichotomous definitions of expertise, experts intubated the term, but not preterm, manikin faster than novices. The experiential definitions of novice and expert used here are inadequate to characterize procedural skill in intubating manikins. Expertise may be better defined by procedural speed and accuracy.
.png)
.png)