Emergency Medicine
Session: Emergency Medicine 3: Serious Bacterial Infections
93 - Aronson Score Performance Among Febrile Infants 29-60 Days of Age
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 93
Publication Number: 93.1476
Publication Number: 93.1476

Kelsey Allen, MD, MPH (she/her/hers)
Assistant Professor
Emory University School of Medicine
Decatur, Georgia, United States
Presenting Author(s)
Background: The Aronson score is an ED-based rule that found, among well-appearing febrile infants <=60 days of age, the following factors were associated with the presence of invasive bacterial infection (IBI: bacteremia and/or bacterial meningitis): age < 21 days, highest ED temperature, abnormal urinalysis, and absolute neutrophil count (ANC). Though the Aronson score has undergone external validation, it has not been evaluated more narrowly in infants beyond four weeks of age, a population for which it is most clinically applicable.
Objective: In keeping with the most recent febrile infant guideline from the AAP, we chose to look at infants >=29 days rather than Aronson’s 21 day cutoff. Given the lower incidence of IBIs in infants between 29-60 days of age, this study sought to apply the Aronson score to this age range to assess its utility for stratifying infants already less likely to undergo a full septic work-up.
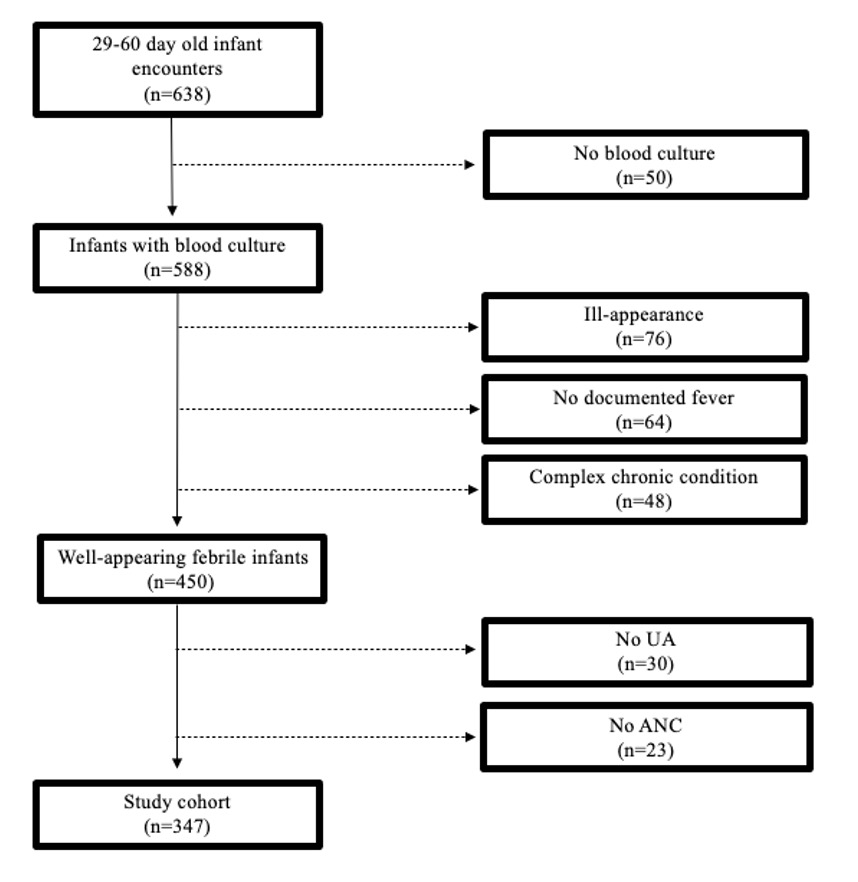
Design/Methods: We conducted a cross-sectional study of infants 29-60 days of age who presented to an academic pediatric ED from July 2011 to December 2018. Afebrile infants (no measured temperature >=38.0 C), those with no blood culture obtained, were ill-appearing, had a complex chronic condition, or were missing any components of the Aronson score were excluded. The primary outcome of IBI was defined by culture growth of a bacterial pathogen. The Aronson score was evaluated using metrics of diagnostic accuracy at previously derived thresholds.
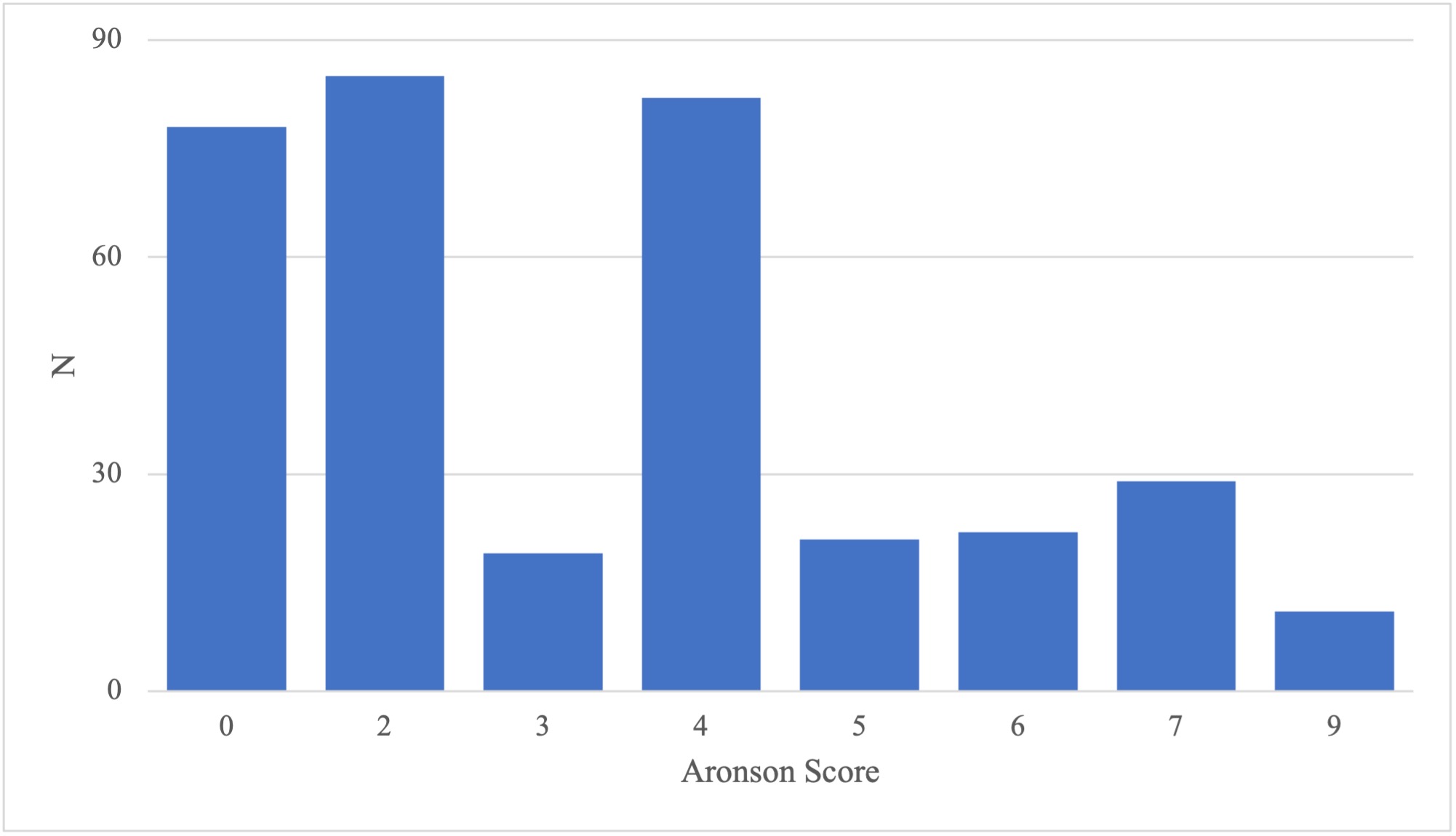
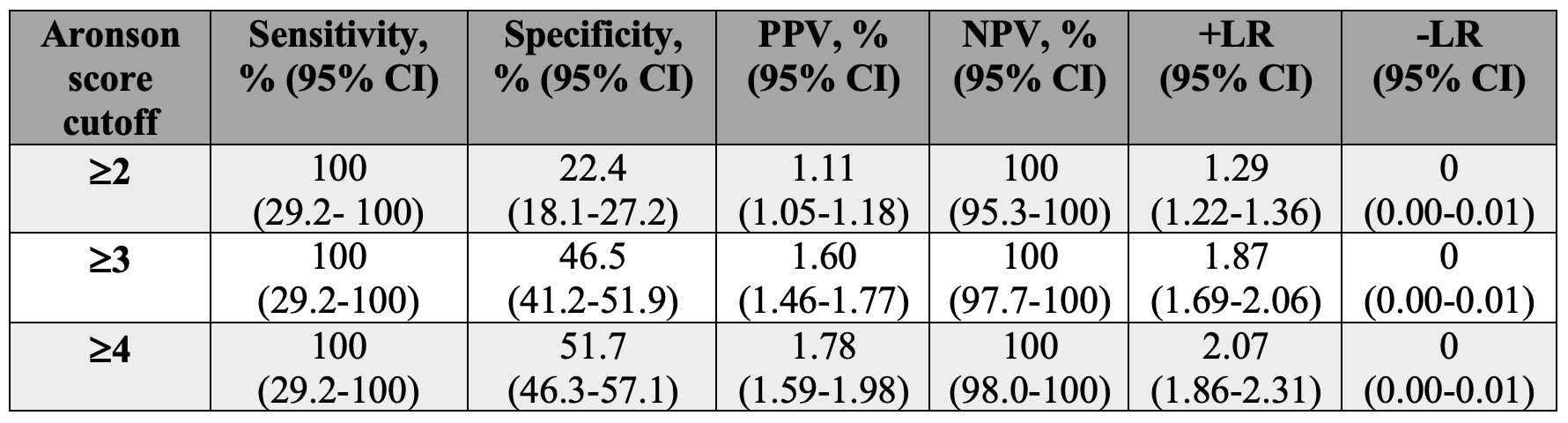
Results: We screened 638 potential subjects, and after exclusions, analyzed 347 well-appearing febrile infants. Three (0.9%) were diagnosed with an IBI (all bacteremia without meningitis). Each infant with IBI had an Aronson score of at least 5. While Aronson score cutoffs of 2-4 had identical 100% sensitivities (100%, 95% CI 29.2-100) and negative likelihood ratios (0, 95% CI 0.00-0.01), specificity (51.7%, 95% CI 46.3-57.1), positive predictive value (1.78, 95% CI 1.59-1.98), negative predictive value (100%, 95% CI 98.0-100%), and positive likelihood ratio (2.07, 95% CI 1.86-2.31) were optimal at a cutoff of 4.
Conclusion(s): Our findings indicate that, at higher score cutoffs, the Aronson score accurately stratifies 29-60 day well-appearing febrile infants as low risk for IBI, which could further obviate the need for lumbar puncture in this older infant age group.