Neonatology
Session: Neonatal General 2: NICU Care Strategies
69 - Improving Survival at Quaternary Care NICUs Following Necrotizing Enterocolitis Totalis, a Condition Previously Considered 100% Lethal.
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 69
Publication Number: 69.220
Publication Number: 69.220

Irfan Ahmad, MD
Clinical Professor
CHOC Children's Hospital of Orange County
Children's Hospital of Orange County
Orange, California, United States
Presenting Author(s)
Background: Necrotizing enterocolitis totalis (tNEC) is a severe form of necrotizing enterocolitis that involves ischemia and necrosis of most of the bowel. The diagnosis is usually made by the surgeon during an exploratory laparotomy. Because tNEC historically has been considered 100% lethal, comfort care is most often offered to the family. However, there are documented cases of survivors of tNEC. Recent growing utilization of intestinal rehabilitation programs (IRP) & improved neonatal parenteral nutrition made us question if tNEC survival is associated with the presence of an IRP.
Objective: To determine if survival and longer lengths of stay among infants with tNEC are associated with the presence of an institutional IRP.
Design/Methods: The Children’s Hospital Neonatal Database (CHND), which includes a collaboration of 45 level IV NICUs, was queried for infants admitted between 1/1/2010 and 12/31/2022. Infants were included if they had a diagnosis of tNEC made at exploratory laparotomy or autopsy during the study period. Survival and median length of stay (LOS) of survivors and non survivors were compared between CHND sites with and without IRPs using nonparametric analysis.
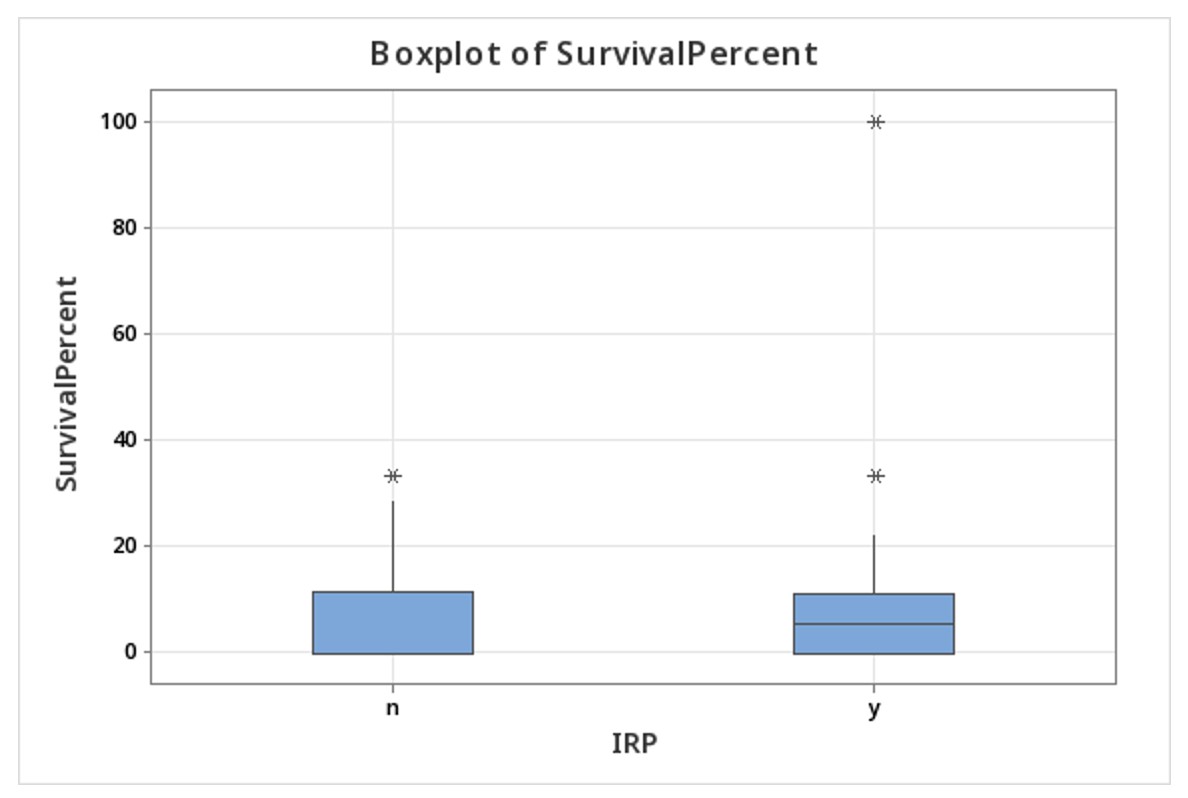
Results: Out of 282,754 infants admitted to 45 centers, there were 633 cases of tNEC reported from 41 centers, 31 of which had an IRP. Thirty-six infants (6% of tNEC), survived to discharge or transfer (Table 1). NICU LOS was (median [IQR]) 78[39-168] vs. 2[2-4] days for survivors vs. non-survivors, (p=0.000). There was at least one survivor in 16/31 (52%) centers with an IRP as compared to 3/10 without IRP (Figure 1). The survival percentage at any given center was [median(range)] 5.4(0-100) at centers with an IRP as compared to 0(0-33) at centers without an IRP (Fig 3; p=ns).
Conclusion(s): Data from this multicenter cohort of quaternary referral centers confirms that tNEC is no longer a uniformly lethal condition. Although the presence of an IRP was not associated with a statistically significant survival difference, the improvement supports the accepted practice of ethically permissible life sustaining therapy. We could not assess the association of intestinal transplant with survival, because the CHND database tracks data to 1 year of age or hospital discharge whereas transplants usually occur when the infants are older. Our data shows an increasingly optimistic prognosis for tNEC, perhaps driven by improved neonatal parenteral nutrition, surgical techniques and the availability of IRPs at quaternary level NICUs.
.jpg)
.jpg)