Global Neonatal & Children's Health
Session: Global Neonatal & Children's Health 2
494 - Risk Factors of Hypoxic Ischaemic Encephalopathy in India: A Health System Perspective
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 494
Publication Number: 494.281
Publication Number: 494.281

Pallavi Muraleedharan, BSN, MHA (she/her/hers)
PhD Student
Imperial College London
London, England, United Kingdom
Presenting Author(s)
Background: The incidence of hypoxic ischemic encephalopathy (HIE) is 10 to 20 times higher in low- and middle-income countries (LMICs) compared to high-income countries. Examining the role of health systems is crucial in understanding the risk factors of HIE, the exact cause of which remains largely elusive. The role of health systems in the incidence of HIE in LMICs, especially in India, is not well explored.
Objective: To determine the health system-specific factors along with other clinical risk factors of HIE in two southern states of India.
Design/Methods: This was a hospital-based unmatched case-control study, nested within a large prospective cohort study. Mother-baby dyads of ≥35 weeks gestation were recruited between March and October 2022. Babies who were depressed at birth and needed resuscitation with assisted ventilation were screened for HIE, using structured neurologic examination between 1 to 6 hours of age. 155 cases were consecutively recruited, along with 259 healthy controls born before or after the case. Data analysis was done by bivariate logistic regression, followed by multivariable logistic regression with a hierarchical approach, using STATA.
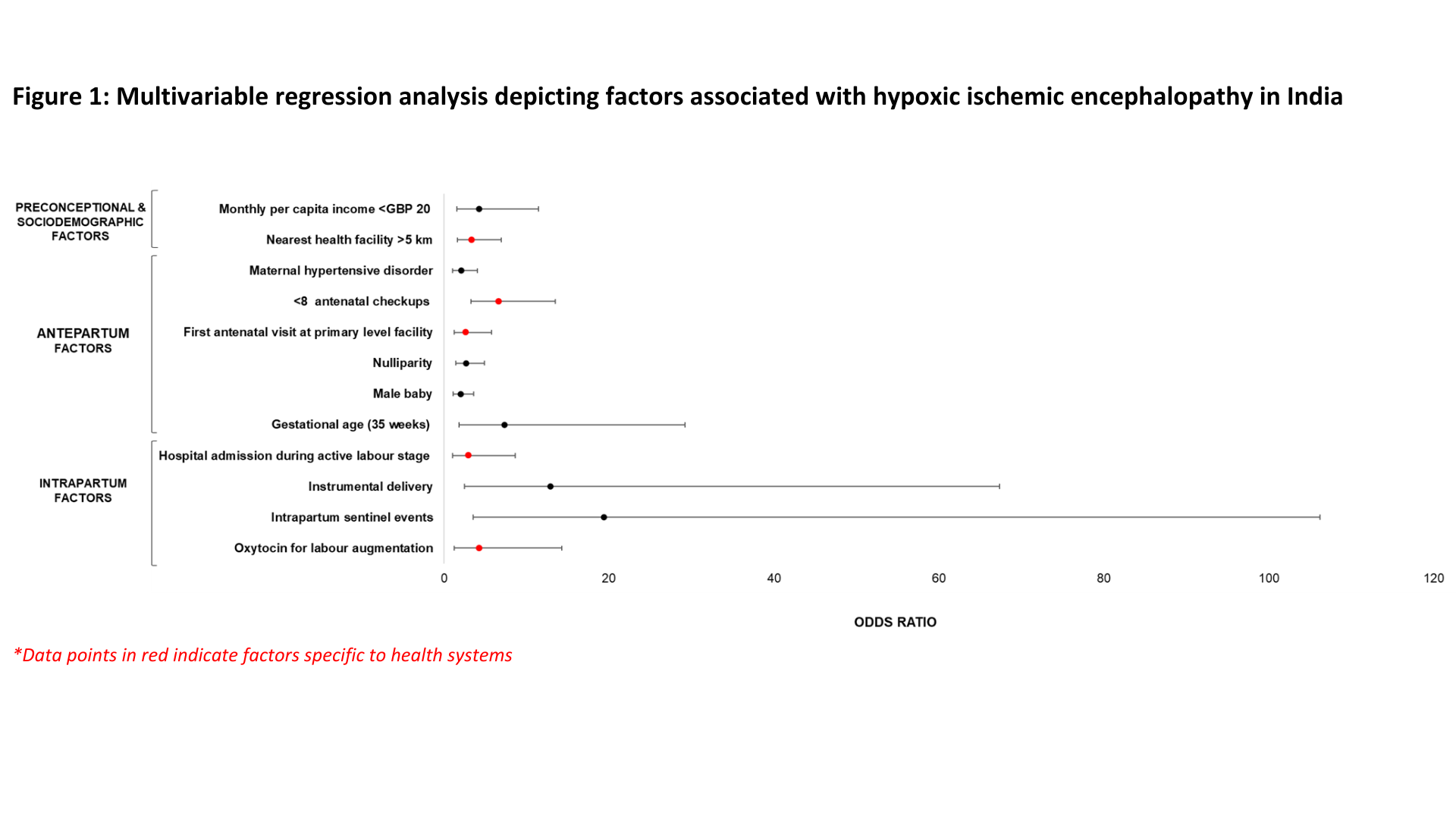
Results: 12 independent risk factors of HIE were identified, of which 5 were specific to health systems, with those related to healthcare service delivery and access predominant (figure 1). The independent risk factors were low monthly per capita income (aOR 4.3; 95% CI 1.6 - 11.5), distance from residence to the nearest healthcare facility being >5 km (aOR 3.4; 95% CI 1.6 – 7.0), ), < 8 antenatal visits by the mother during pregnancy (aOR 6.7; 95% CI 3.3 - 13.5), commencing the ANC check-ups at a facility without emergency obstetric services (aOR 2.7; 95% CI 1.2 - 5.8), maternal hypertensive disorder (aOR 2.1; 95% CI 1.1 - 4.1), nulliparity (aOR 2.7; 95% CI 1.5 - 4.9), male baby (aOR 2.0; 95% CI 1.2 - 3.6), gestational age of 35 weeks (aOR 7.4; 95% CI 1.9 - 29.2), admission to the hospital during active stage of labour (aOR 3.0; 95% CI 1.0 - 8.6), instrumental delivery (aOR 12.9; 95% CI 2.5 - 67.4), intrapartum sentinel events (aOR 19.4; 95% CI 3.6 - 106.2), and use of oxytocin for augmentation of labour (aOR 4.3; 95% CI 1.3 - 14.3).
Conclusion(s): This study shows that health system factors are associated with HIE along with other antepartum and intrapartum factors in India. A well-performing health system can potentially reduce the incidence of HIE through the provision of good-quality antenatal and intrapartum care in LMICs.