Immunizations/Delivery
Session: Immunizations/Delivery 1
38 - The Impact of Virtual Reality Simulation Training on COVID-19 Vaccination Rates: A Mixed Methods Pilot Study
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 38
Publication Number: 38.1425
Publication Number: 38.1425

Francis Real, MD, MEd (he/him/his)
Associate Professor of Pediatrics
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: The COVID-19 vaccine is recommended for adolescents, yet only 72% of U.S. adolescents have received at least one dose. We developed a simulation-based virtual reality (VR) intervention, co-created with community members, to train clinicians in recommending and addressing COVID-19 vaccine hesitancy using motivational interviewing (MI) skills. The intervention included real-time interactions with virtual avatars driven by a human facilitator who provided coaching to participants.
Objective: To assess the efficacy of a clinician-focused VR intervention on COVID-19 vaccination rates and to identify clinician-level facilitators and barriers to implementing communication strategies in clinical practice.
Design/Methods: We recruited clinicians practicing at an adolescent primary care clinic located within a large, urban academic medical center to participate in the VR intervention in September 2022. The change in vaccination rates was assessed among participants using an interrupted time series design with the pre- and post-intervention periods defined as the three-months prior to and following training, respectively. We also assessed for billing practices related to COVID-19 vaccine counseling behaviors. Chi-square test was used to test for differences in COVID-19 vaccination rates and billing practices. A subset of participating clinicians underwent individual implementation interviews in March 2023. Interview data was recorded, transcribed, and analyzed using the Rapid and Rigorous Qualitative Data Analysis technique.
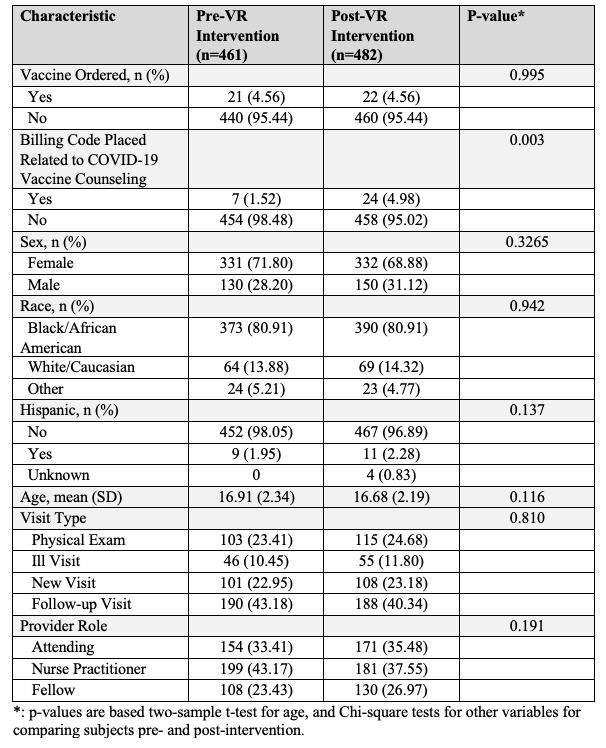
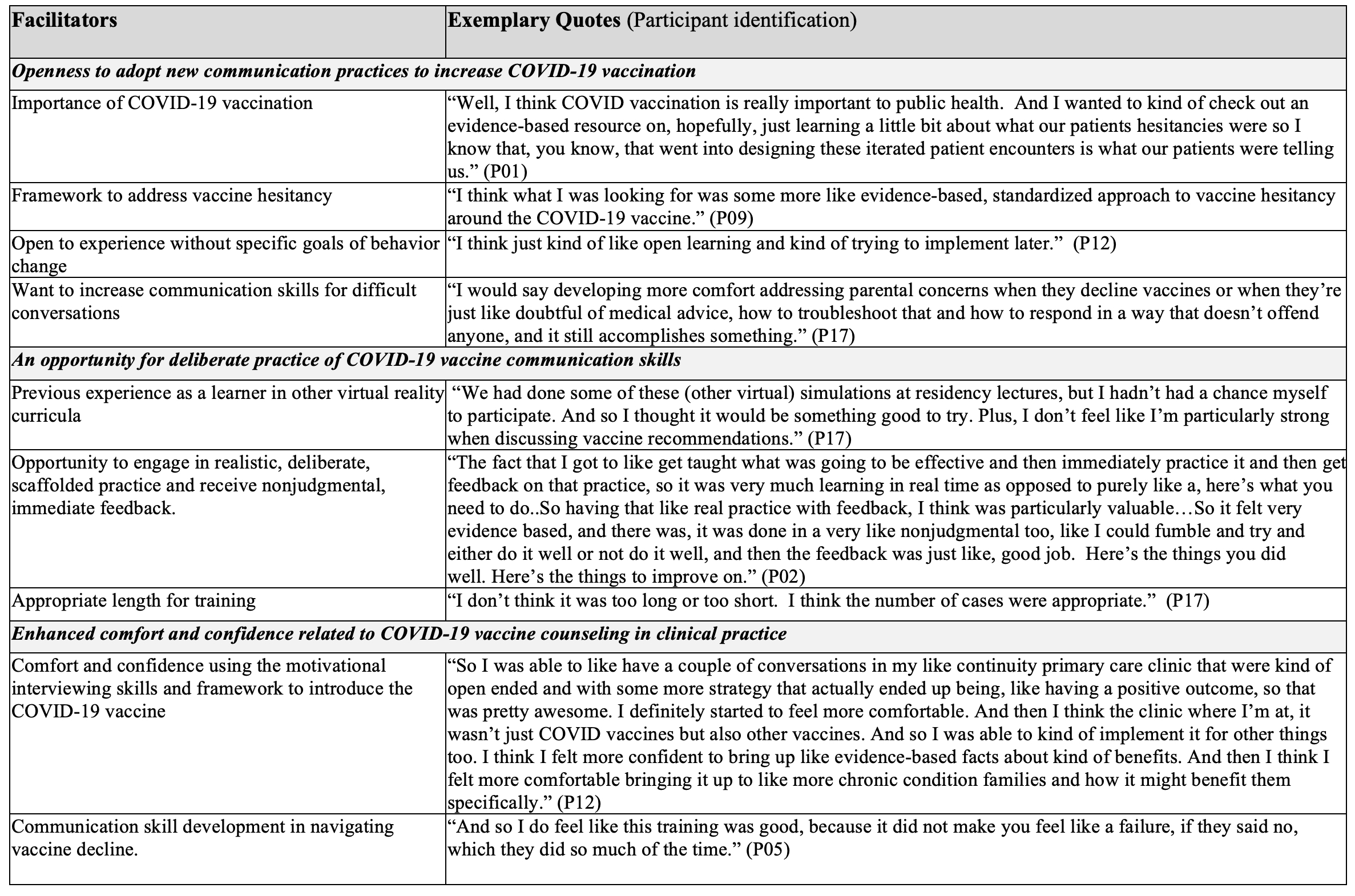
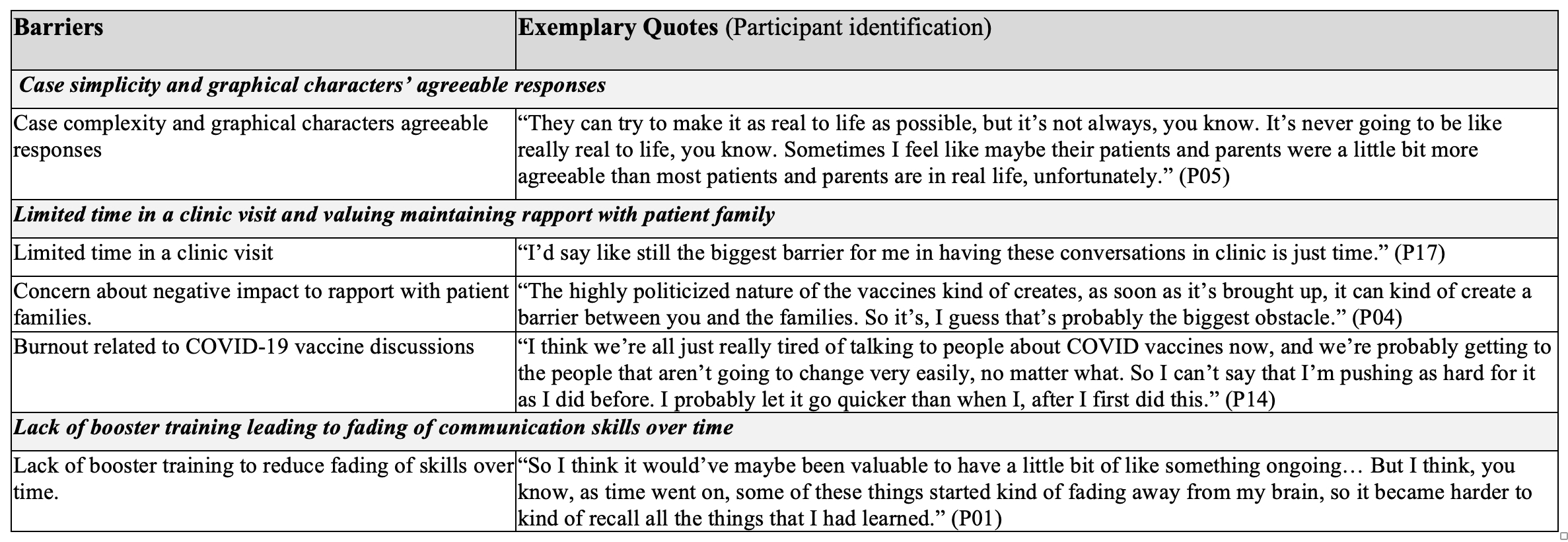
Results: A total of 19 clinicians (46% of eligible clinicians) completed the intervention. The majority were female (68.4%), White (78.9%), and Non-Hispanic (100%). There was no change in patients’ COVID-19 vaccine initiation rates post-training. There was a statistically significant increase in billing for vaccine counseling (1.5% to 5.0%; p=0.003) (Table 1). Nine participants enrolled in the interviews. Though participants indicated an openness to adopt new COVID-19 vaccine communication skills and appreciated an opportunity for practice, identified barriers to implementation of skills in clinical practice included limited time, concerns of negatively impacting rapport, fatigue related to vaccine discussions, and fading of skills over time (Table 2/3).
Conclusion(s): COVID-19 vaccine initiation did not increase following VR training though billing for time spent counseling increased. Modifications to the intervention might include emphasizing strategies to provide efficient counseling and booster training to support skill retention.