Breastfeeding/Human Milk
Session: Breastfeeding/Human Milk 1: Breastfeeding
471 - Birth hospital breastfeeding patterns among infants with prenatal opioid exposure
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 471
Publication Number: 471.1925
Publication Number: 471.1925

Jennifer McAllister, MD (she/her/hers)
Associate Professor
Cincinnati Children's Hospital
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Breast milk is the optimal nutrition for newborns, and infants with prenatal opioid exposure (POE) who receive breast milk are at decreased risk of symptoms and pharmacologic treatment for withdrawal, have shorter length of hospital stay, and have increased maternal bonding and attachment. Breastfeeding is generally recommended for mothers who discontinue nonprescribed substance use by the time of delivery, however rates of infants with POE who receive breastmilk are lower than those without POE, and there is limited information about breastfeeding patterns during the birth hospitalization.
Objective: To describe breastfeeding patterns during the birth hospitalization in infants with POE compared to those without POE.
Design/Methods: We utilized the Maternal Infant Data Hub (MIDH), which is a regional perinatal data repository of maternal and infant data of dyads born within a large academic hospital system. Infants born between 2017-2019 were included. POE was identified based on universal maternal urine toxicology testing at delivery hospitalization, newborn toxicology testing, maternal diagnosis code of opioid use disorder during pregnancy, and/or newborn diagnosis code of POE. Feeding patterns were collected and analyzed according to any and only breast milk feedings, first feeding, and feeding at discharge Descriptive statistics and chi-squared or Fisher’s exact test were to examine the relationship between feeding variables and POE.
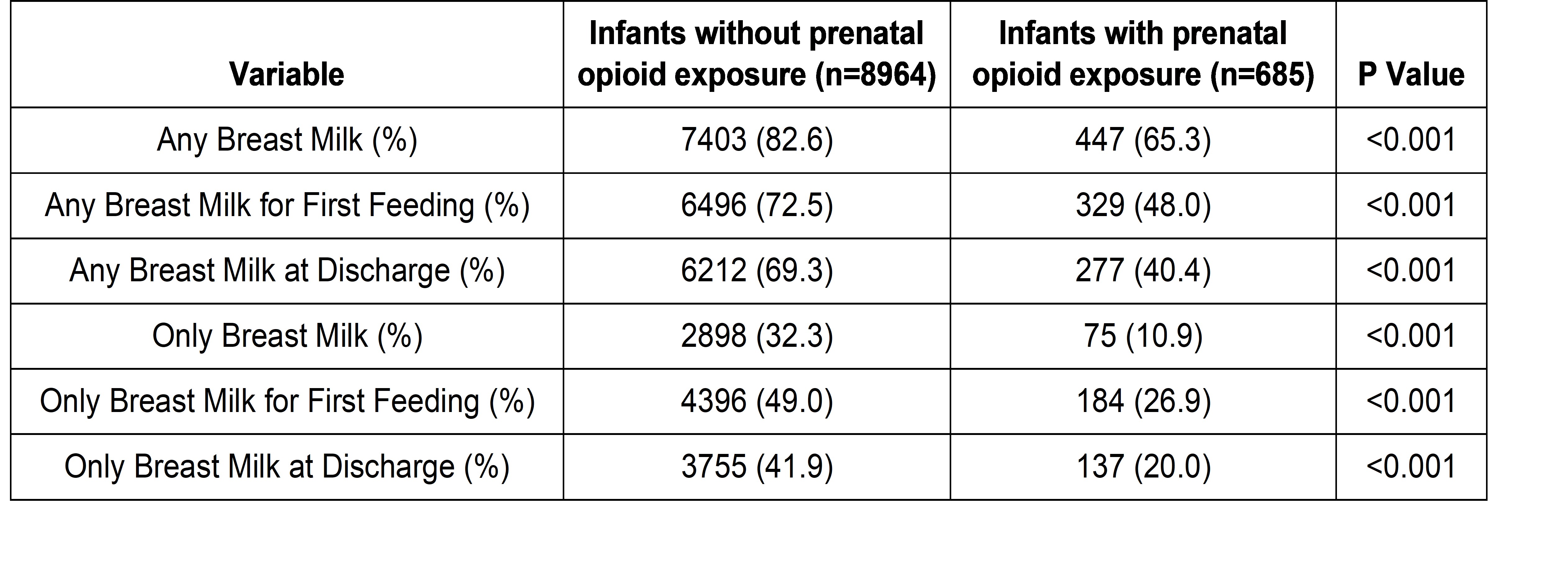
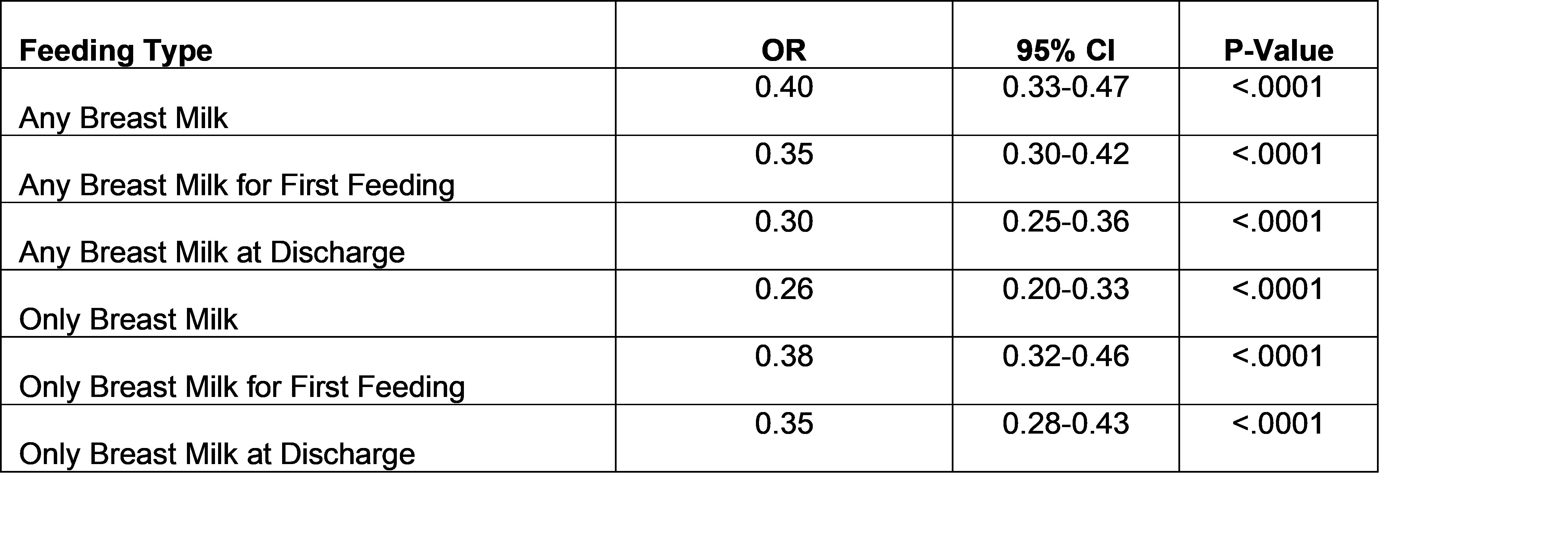
Results: There were 9649 children included in our study. Of those, 685 (7%) had POE. Among infants with POE, 65.3% received any breast milk and 10.9% exclusively received breast milk compared to 82.6% and 32.3% respectively in infants without POE during the birth hospitalization. Additionally, infants with POE had considerably lower odds of having their first feed as breastmilk, to be receiving any breast milk at discharge, or exclusive breast milk at discharge.
Conclusion(s): Breastfeeding is important and recommended for infants with POE providing significant benefits for both the mother and infant. Our study demonstrated infants with POE are less likely to start and continue to receive breastmilk during birth hospitalization compared to those without POE. Further work is needed to understand reasons for lower hospital breastfeeding rates including potential systemic biases, lack of breastfeeding support, and feeding problems or weight loss specific for this population.