Health Services Research
Session: Health Services Research 4: Population Monitoring and Management
247 - Differences in Healthcare Utilization, Complications and Procedures among Privately and Publicly Insured Children with Sickle Cell Anemia
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 247
Publication Number: 247.1944
Publication Number: 247.1944

Melissa Plegue, MA (she/her/hers)
Statistician Expert
University of Michigan Medical School
Ann Arbor, Michigan, United States
Presenting Author(s)
Background: Children with sickle cell anemia (SCA) face serious morbidities, leading to numerous acute, routine, and preventive healthcare encounters. Children on public insurance often have decreased access to high quality care. Little is known regarding the impact of insurance type on the breadth of healthcare and services received within the SCA population.
Objective: Compare characteristics of annual healthcare utilization among children with SCA insured by Medicaid versus those privately, such as encounter type, rates of SCA-related complications, and presence of SCA management procedures.
Design/Methods: Individuals with SCA were identified using validated case definitions from the Merative MarketScan Commercial and Multi-State Medicaid Databases (2009-2019). Annual claims for individuals 1-17 who were continuously enrolled for 365 days were extracted. Healthcare encounters were identified as distinct service dates and categorized hierarchically as inpatient, emergency department (ED), outpatient, procedure, laboratory visit, or radiology. Diagnosis and procedure codes were used to identify instances of select SCA-related complications (e.g. stroke, acute chest syndrome) and procedures (e.g. vaccinations, transfusions). The probability of having >=1 encounter type, complication, or procedure in a year was estimated and compared between insurance groups using logistic regression models. Average number of encounters, overall and by type, were compared between groups using linear mixed models. All models accounted for multiple claim-years within a person and were estimated with insurance type as main covariate of interest.
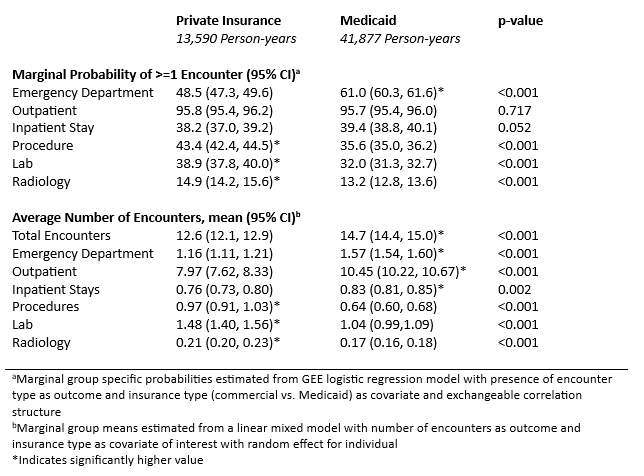
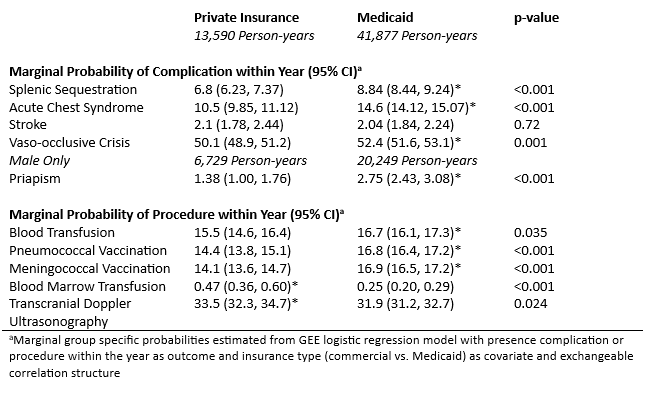
Results: 13,092 individuals with SCA contributed 55,467 person-years of data; 68.6% of individuals and 75.5% of person-years were Medicaid enrollees. Average number of annual encounters for individuals on Medicaid was 14.7, significantly higher than private insurance (12.6, p< 0.001). Medicaid enrollees had higher average ED, outpatient and inpatient encounters, however, significantly lower procedure, laboratory and radiology visits (Table 2). Medicaid enrollees had significantly higher rates of complications, apart from stroke, compared with those on private insurance, and higher rates of vaccination and blood transfusions (Table 3).
Conclusion(s): Compared to children with SCA enrolled in private insurance, those enrolled in Medicaid have higher levels of healthcare encounters and SCA-related complications, but lower number of procedural, laboratory and radiology visits. Targeted interventions are needed to address social determinants of health among children with SCA enrolled in Medicaid.
.png)