Neonatology
Session: Neonatal Neurology 4: Clinical
528 - Comprehensive Neurocritical Care in Extremely Low Birthweight Preterm Infants: An Integrated Monitoring of Cerebral Perfusion, Cardia Output and Brain Images
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 528
Publication Number: 528.1501
Publication Number: 528.1501
Kai-Hsiang Hsu, MD
Associate Professor of Pediatrics
Chang Gung Memorial Hospital, Linkou
Taipei, Taipei, Taiwan (Republic of China)
Presenting Author(s)
Background: Abnormal regional cerebral saturation (rcSO2) is a risk related to neurologic injury in extremely preterm infants.
Objective: To study if implementation of a neurocritical care bundle involving rcSO2, cardiac output (CO) monitors and functional echo (fEcho) would contribute to the management of cerebral hemodynamic disturbances and secure neurologic outcomes in preterm infants.
Design/Methods: This is a prospective study enrolling preterm infants of gestation age (GA) ≤28 weeks or birthweight (BW) ≤1000 g except those with a significant anomaly or perinatal asphyxia. Monitoring devices included near-infrared spectroscopy for rcSO2, brain fEcho for measuring cerebral blood flow (CBF) and screening intraventricular hemorrhage (IVH), and electrical cardiometry (EC) for assessing CO. The monitoring protocol included continuous NIRS+EC plus daily fEcho within the first 72 hours of life, followed by weekly assessments in the first month and monthly assessments until discharge or term-equivalent age (TEA) (Fig 1). Cerebral hypoxia was defined as rcSO2 < 55%. Fraction of tissue oxygen extraction (FTOE) was calculated according to rcSO2 and arterial saturation (SaO2), with a reference range of 10%–40%. An algorithm was implemented to maintain rcSO2 and FTOE within target ranges (Fig 2). Brain magnetic resonance imaging was obtained at TEA for structural evaluation. Poor neurologic outcomes were defined as mortality, IVH grade ≥2, periventricular leukomalacia (PVL), ventriculomegaly or electroencephalogram-confirmed seizure.
Results: A total of 30 extremely preterm infants (GA 27.1±2.0 weeks, BW 830±225 g) were enrolled. There was no substantial alteration of rcSO2, SaO2, FTOE and CO (per kg) from birth to TEA in individuals, but CBF increased with post-natal age. Mean rcSO2 was 71.0±10.6 % and FTOE was 25.2±11.1 %. Seven infants were with poor neurologic outcomes (4 infants died (2 of them also had grade 4 IVH), 2 others had grade 2 IVH, and 1 developed PVL). Generally lower rcSO2 and higher FTOE were seen in infants with poor neurologic outcomes, and a regression analysis revealed that lower BW and the occurrence of cerebral hypoxia were independent risk factors. Comparing to the control cohort, the study group demonstrated a higher likelihood of intact neurological outcome among infants who had already been discharged (21/28 of the study group vs. 22/46 of the cohort, p=0.029) (Fig 3).
Conclusion(s): Using multidiscipline hemodynamic monitors and a management algorithm to safeguard rcSO2 is clinically feasible. The study will continue to assess the long-term impacts on neurodevelopmental outcomes.
.jpg)
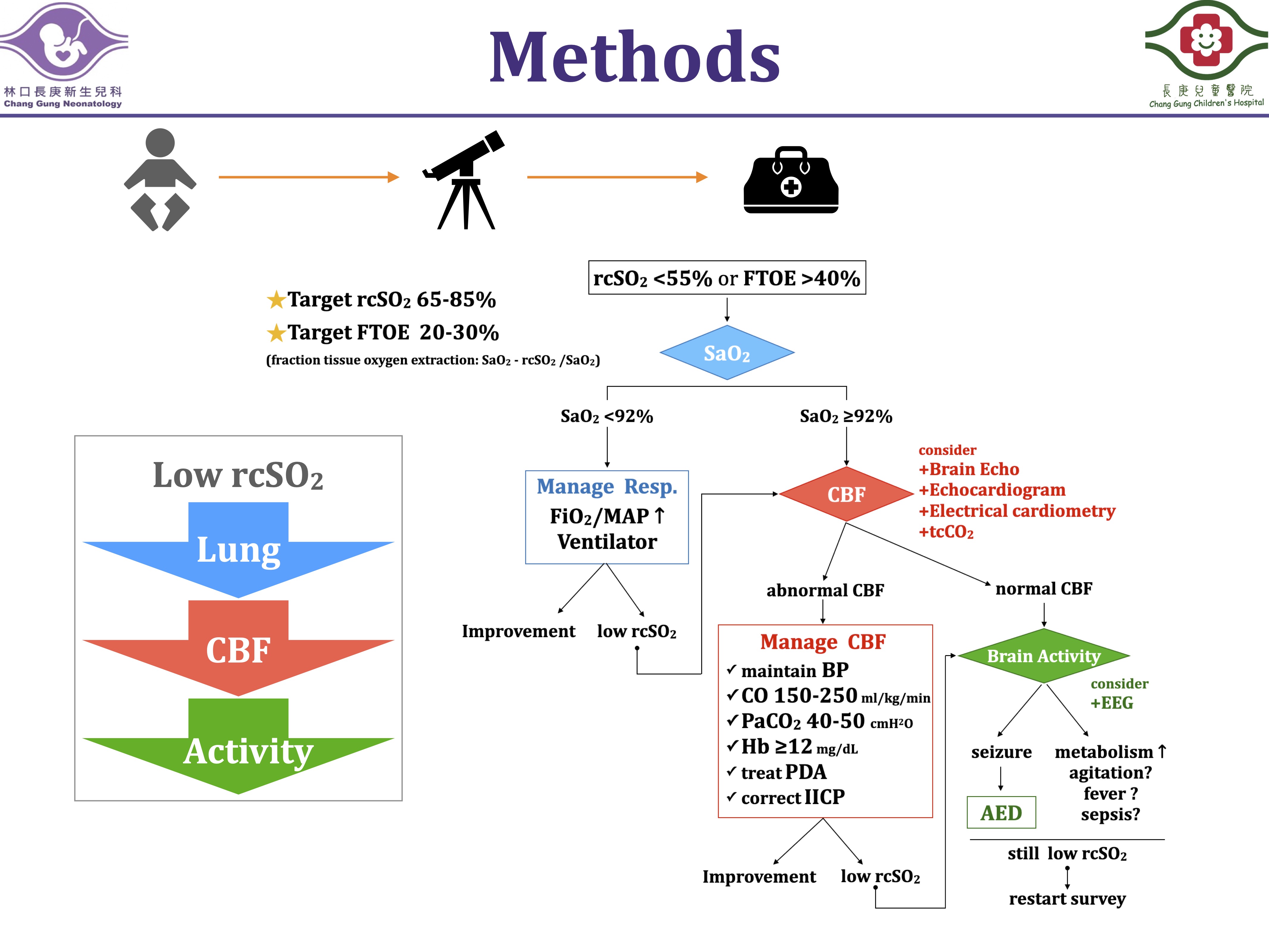
Figure 3.jpeg
