Neonatology
Session: Neonatal/Infant Resuscitation 1
263 - Premedication for endotracheal intubation in the delivery room - Can we avoid bradycardia?
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 263
Publication Number: 263.3186
Publication Number: 263.3186
- MK
Mary Divya Kasu, MD
Fellow
Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo
Buffalo, New York, United States
Presenting Author(s)
Background: Preterm infants are at higher risk of needing endotracheal intubation in the delivery room. Desaturations and bradycardia are common complications associated with endotracheal intubation. Bradycardia associated with endotracheal intubation is presumed to be vagal in origin and is not prevented by preoxygenation and the avoidance of hypoxemia. Previous studies have shown that nasal cannula could decrease desaturation episodes but not bradycardia. Since heart rate (HR) is a marker for resuscitative steps, using intramuscular (IM) atropine could reduce the incidence of bradycardia. Atropine is an anticholinergic agent that can be administered IM and used as a premedication for intubation in the delivery room. Since it takes at least 30 seconds to intubate, our goal was to use 1mg atropine IM before intubation to ensure that the HR did not drop in a preterm model.
Objective: To evaluate if 1mg IM atropine will help sustain the HR if it is < 100 bpm before endotracheal intubation for at least a minute.
Design/Methods: Preterm lambs (126-129d) were instrumented while on placental circulation. Post instrumentation, the lambs were delivered with an occluded airway until HR was < 100 bpm. Atropine (1mg) or placebo (1mg/2.5cc) was given via IM route to the study and control group before intubation to understand if HR was sustained, respectively. We monitored the HR and hemodynamic variables for at least 2 min before endotracheal intubation and positive pressure ventilation (PPV). Endotracheal intubation was performed after this while monitoring the heart rate.
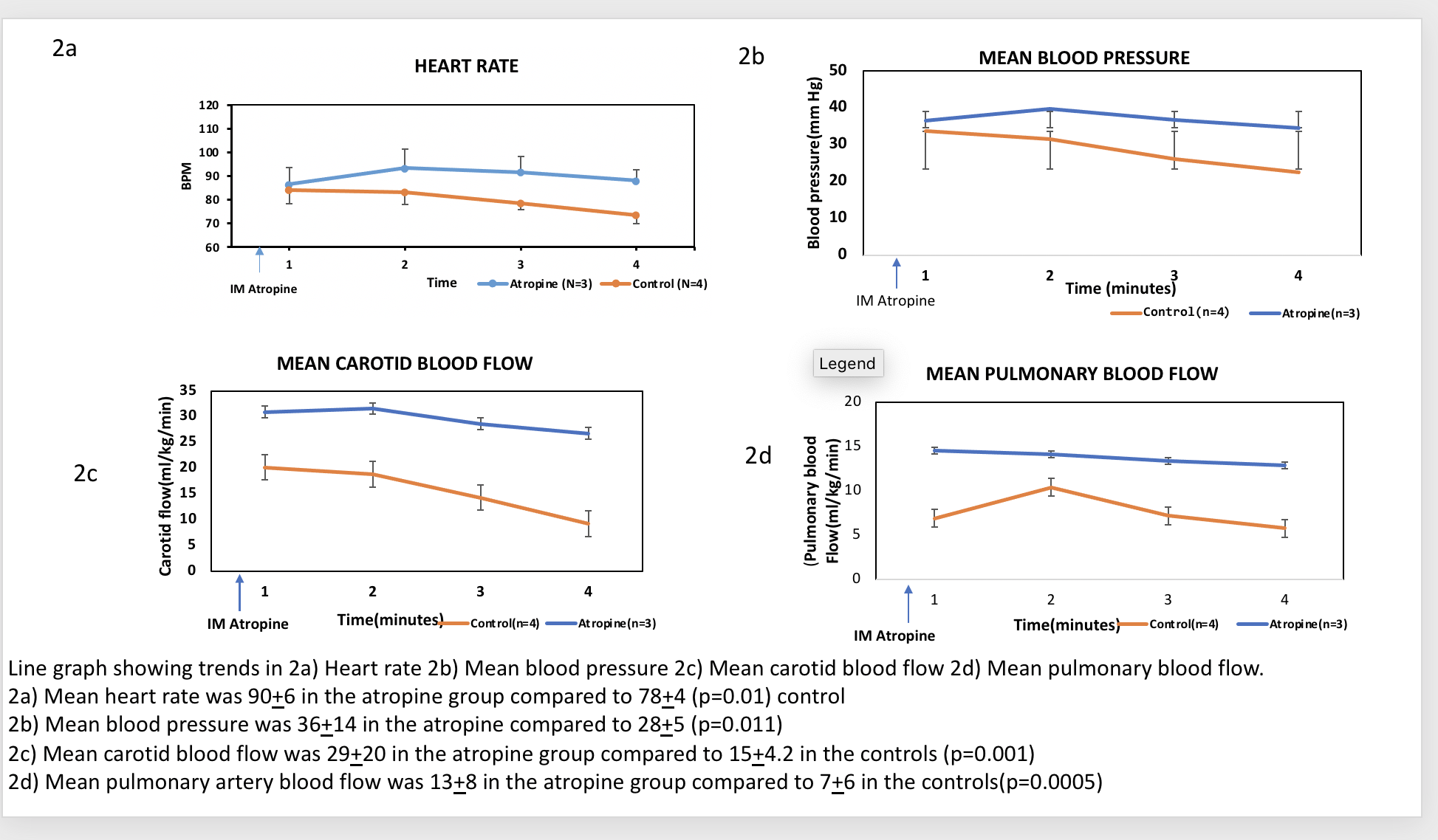
Results: A total of 7 asphyxiated preterm ovine lambs were used, 4 in controls and 3 in the study group. Post atropine administration during endotracheal intubation, the heart rate was 90+/-6 bpm in the atropine group compared to 78+/-4 bpm in the control group (p value=0.01) (fig 2a) before endotracheal intubation. Preductal saturations were also higher in the study group compared to control. Mean blood pressure, carotid blood flow, and pulmonary blood flow were all significantly higher in the atropine group compared to the controls (fig 2b, 2c, 2d) (p value= < 0.05).
Conclusion(s): In the preterm asphyxiated lamb model after birth and asphyxia, atropine administration before endotracheal intubation led to sustained HR and significantly higher hemodynamic parameters during and post endotracheal intubation compared to controls. Since atropine is part of premedication for non-emergent endotracheal intubation as recommended by AAP COFN, our findings could be translated to bedside in the delivery room and lead to a lower incidence of bradycardia.
.png)