Neonatology
Session: Neonatal General 7: Respiratory
248 - Evaluation of an Extubation Criteria for Preterm Infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 248
Publication Number: 248.3231
Publication Number: 248.3231

Melody Chiu, MD (she/her/hers)
Clinical Fellow
University of Texas Southwestern Medical Center
Dallas, Texas, United States
Presenting Author(s)
Background: Prolonged mechanical ventilation and extubation failure are associated with higher incidence of bronchopulmonary dysplasia (BPD), neurodevelopmental impairment, and mortality among preterm infants. Currently, optimal extubation criteria and the role of a predefined criteria in decreasing duration of mechanical ventilation, extubation failure, and adverse clinical outcomes have not been established.
Objective: To select an extubation criteria from published literature and compare characteristics and outcomes of preterm infants who are categorized based on meeting an a priori extubation criteria and timing of extubation.
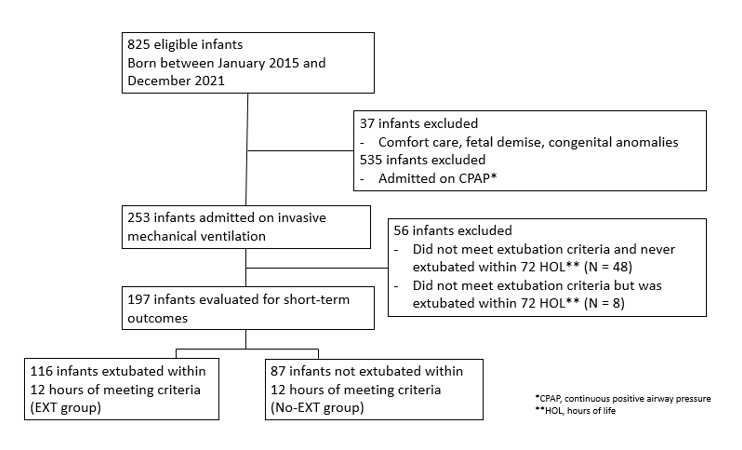
Design/Methods: This was a single center retrospective study that included preterm infants born at < 30 weeks’ gestational age (GA) and admitted to a tertiary NICU between January 2015 to December 2021. Infants were classified into 2 groups: those who met an a priori extubation criteria and were extubated within 12 hours of meeting criteria (EXT) and infants who met criteria but were not extubated within 12 hours (No-EXT). Maternal and neonatal factors were compared between the 2 groups. Primary outcome was duration of mechanical ventilation in hours, and secondary short-term outcomes included extubation failure (need for re-intubation after 5 days), moderate-severe BPD, death, length of stay, pneumothorax, pulmonary hemorrhage, and pulmonary interstitial emphysema (PIE). A subset of clinical outcomes was also adjusted based on GA.
Results: Of the 197 infants who met inclusion criteria, 116 were classified into EXT group, and 81 were classified into No-EXT group. Compared to EXT group, No-EXT group had a lower median GA and birth weight and higher proportion of small for gestational age (SGA). There were no differences in maternal factors. No-EXT group had longer median duration of bradycardia in the delivery room and lower Apgar 1-minute scores. Rates of extubation failure were not statistically significant between the groups. No-EXT group had longer ventilator days and time to first extubation. Furthermore, higher proportion of No-EXT group received high frequency ventilation and developed PIE, pneumothorax, pulmonary hemorrhage, and moderate-severe BPD.
Conclusion(s): Preterm infants not extubated within 12 hours of meeting an a priori criteria were of lower in gestational age and SGA. Infants who were not extubated within 12 hours of meeting extubation criteria are at higher risk of adverse outcomes even after adjusting for GA. Prospective studies comparing predefined extubation criteria are warranted to help reduce duration of mechanical ventilation and adverse respiratory outcomes.
.png)
.png)
