Emergency Medicine
Session: Emergency Medicine 4: Infections
109 - Non-invasive urinary tract infection screening for children 90 days and older in a pediatric emergency department
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 109
Publication Number: 109.1351
Publication Number: 109.1351

Olivia Ostrow, MD (she/her/hers)
Staff Physician and Director of Quality and Safety, Emergency Medicine
Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
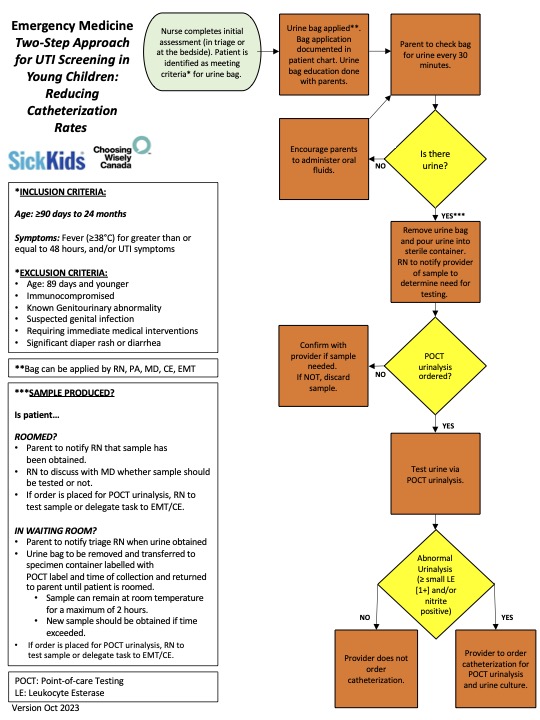
Background: Urinary tract infection (UTI) is a common bacterial diagnosis for children presenting with fever to the Emergency Department (ED). A urine bag UTI screening pathway is a noninvasive technique that has been successfully implemented in our pediatric ED for older infants and children 6-24months of age, however, newer guidelines also endorse non-invasive urine testing for UTI screening in younger febrile infants. While any level of leukocyte esterase (LE) is suggested as a positive screen with the urine bag non-invasive technique, there is limited supporting evidence for this recommendation in infants less than 6 months of age.
Objective: Our aim was to expand the age of children eligible for our noninvasive urine bag UTI screening pathway to include children aged 90 days to 6 months to decrease the number of unnecessary invasive urinary catheterizations by 50% over 12 months without impacting ED length of stay (LOS), return visits (RVs) or missed UTI diagnoses. Our secondary aim was to describe the association between screening UA LE levels and final urine catheter culture results.
Design/Methods: An interprofessional study team was created and engaged key stakeholders. Using the Model for Improvement, a multipronged intervention strategy was developed. The current urine bag screening pathway was updated and implemented using Plan, Do, Study Act (PDSA) cycles using a urine bag sample with Point-of-Care (POC) urinalysis (UA) as a screening approach. The outcome measure was the rate of ED urine catheterizations for aged 90 days to 6 months and balancing measures included ED LOS, RVs, missed UTIs. We also monitored the rate of positive urine cultures in patients based on LE levels on screening UA. Statistical process control methods and descriptive statistics were used for analysis.
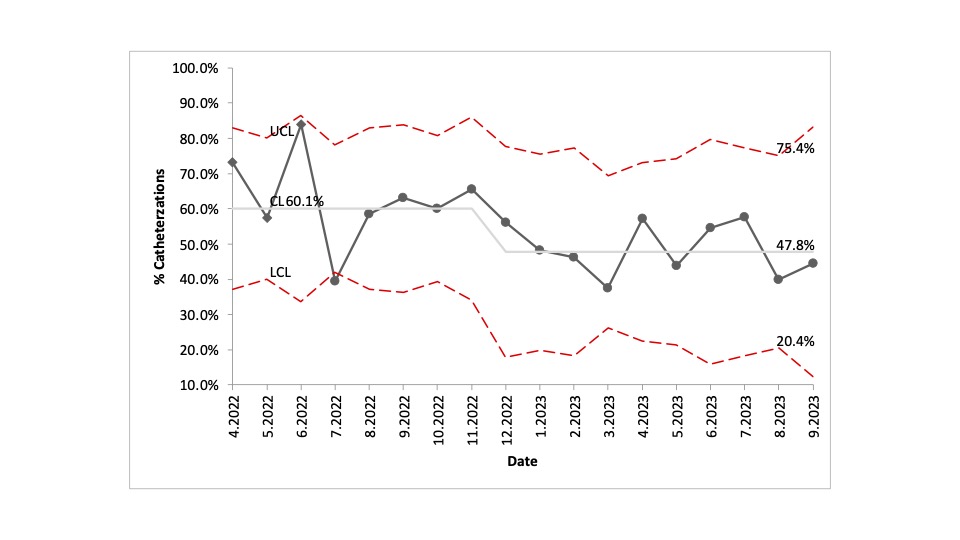
Results: During the study period from April 2022 to September 2023, early analysis demonstrates the ED catheterization rate for included patients decreased from a baseline mean of 60.1% to 47.8%, with no change in ED LOS, RVs or missed UTIs. None of the patients with a trace level of LE (15leu/µL) on screening UA (30.4% of the patients with a positive LE screen), had a positive urine catheter culture.
Conclusion(s): A urine bag screening pathway can successfully be expanded in the ED to decrease unnecessary, invasive catheterization in children 90days and older for UTI screening without change to ED LOS, RVs or missed UTIs. There was also no association between a trace LE level on screening UA and a positive catheter culture suggesting a higher LE screening threshold can be considered.