Neonatology
Session: Neonatal GI Physiology & NEC 2: Enteral Nutrition and Growth
528 - The association of urine sodium and growth in infants with intestinal failure
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 528
Publication Number: 528.2026
Publication Number: 528.2026

Ricci Allen, MD, MSc (she/her/hers)
Categorical Pediatrics Resident
Johns Hopkins Children's Center
Silver Spring, Maryland, United States
Presenting Author(s)
Background: Infants with intestinal failure (IF) are at risk for poor growth and subsequent neurodevelopmental impairment. Sodium depletion is implicated in impaired growth, but the relationship between sodium depletion, sodium supplementation, and growth failure in infants with IF is unclear.
Objective: To determine the association between urine sodium and postnatal growth in infants with IF.
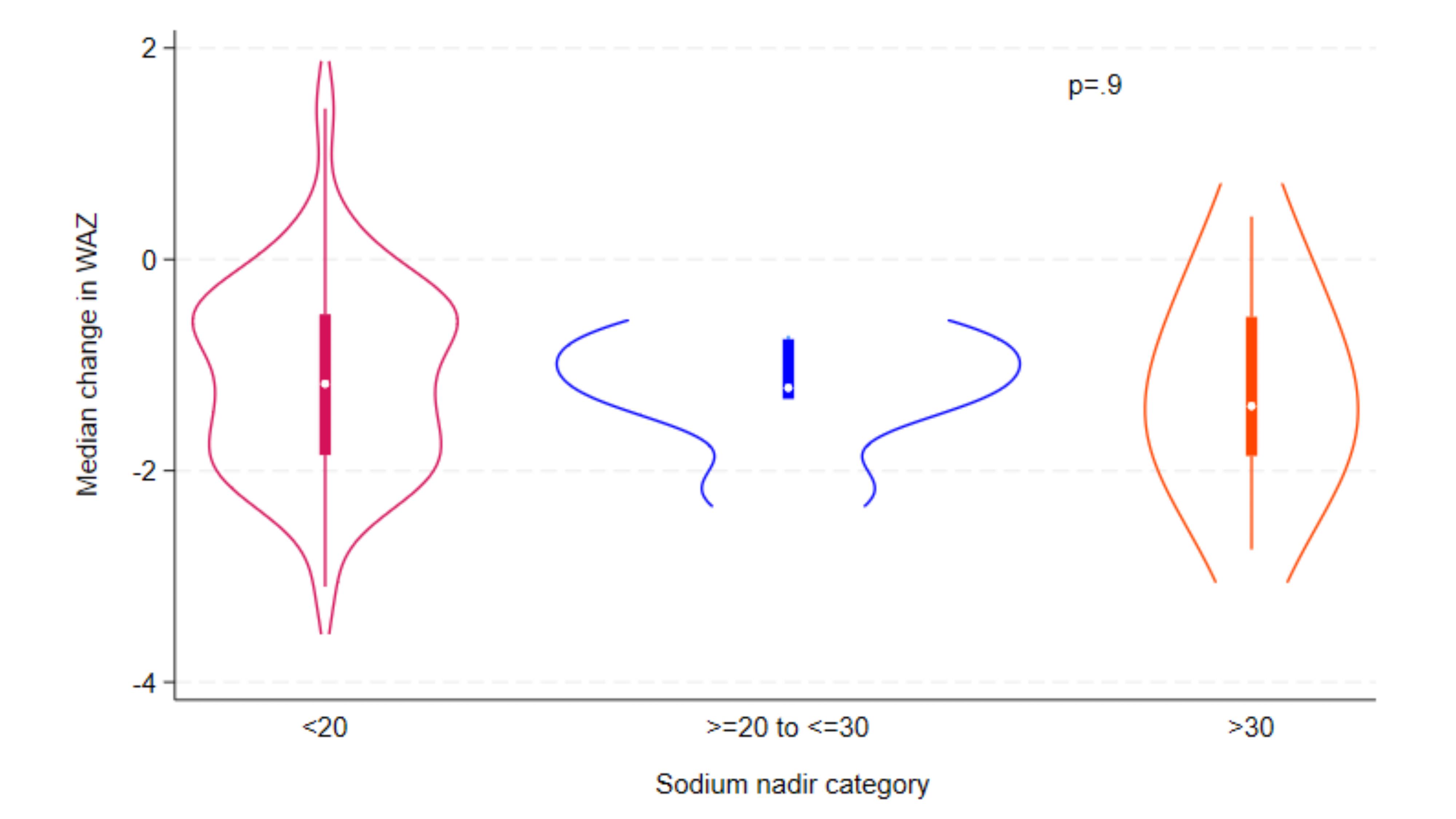
Design/Methods: A retrospective cohort of infants with IF identified at our institution over a five-year period was analyzed. Weekly urine sodium levels are obtained in infants to guide sodium supplementation at this site. Urine sodium nadir prior to post-menstrual age (PMA) of 44 weeks was identified for each infant and considered the primary study exposure. The primary study outcome was the change in weight-for-age z (WAZ) scores between birth and PMA of 44 (+/-2) weeks. Demographic, intestinal injury data, WAZ, and urine sodium levels were assessed with summary statistics. A two-sided Kruskal-Wallis test was used to determine whether differences in WAZ from birth to 44 (+/-2) weeks PMA were associated with categories of urine sodium nadir ( < 20, 20 to 30, >30 mEq/L).
Results: Among 86 eligible infants with IF, 60 (69.8%) had a measured urine sodium level. The cohort was predominantly male (62%) with a median gestational age and birth weight of 31.4 weeks and 1400 grams, respectively. The most common diagnoses leading to IF were necrotizing enterocolitis (27%), gastroschisis (17%), intestinal atresia (15%) and isolated intestinal perforation (11%). Among the total cohort, 75% (n=45) of infants had a urine sodium nadir < 20, 8.3% (n=5) between 20 to 30, and 16.7% (n=10) >30 mEq/L (Figure 1). The median difference in WAZ between birth and PMA of 44 (+/-2) was 1.2 standard deviations (SD). We did not observe a significant association between sodium nadir level and change in WAZ (p=.9).
Conclusion(s): In this single center cohort of infants with IF, over 80% had a urine sodium nadir of < 30 mEq/L, indicating total body sodium deficiency or depletion. Although WAZ decreased from birth to PMA of 44 (±2 wks) by 1.2 SD among this study population, the association between change in WAZ and urine sodium nadir levels did not reach statistical significance at our a priori determined level of .05. For these infants, this could be due to sodium supplementation being guided by urine sodium levels. This data suggests potential benefits for following this non-invasive measurement in this high-risk population. Ongoing analyses will evaluate sodium supplementation and how it modifies the association between urine sodium and growth patterns.