Neonatology
Session: Neonatal Pulmonology - Clinical Science 2: Lung Imaging, Lung Function
207 - Lung Ultrasound Severity Scores and its utility in predicting success of weaning off respiratory support in neonates born premature.
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 207
Publication Number: 207.2972
Publication Number: 207.2972
- AE
Ahmed said Elkordy, MD (he/him/his)
Clinical Fellow
LHSC
London, Ontario, Canada
Presenting Author(s)
Background: Preterm infants often require respiratory support in the newborn intensive care unit. Complete trial off around 30-34 weeks post-menstrual age (PMA) is by trial and error based on clinical and physiological variables. Lung ultrasound (LUS) is a reliable adjunct in the diagnosis and management of most neonatal lung conditions. However, its utility in accessing readiness for successful weaning off respiratory pressure support in preterm neonates has not been explored.
Objective: To determine the utility of LUS severity score (LUS-sc) in predicting successful weaning off of respiratory pressure support after 32weeks CGA in neonates born ≤32 weeks gestational age (GA).
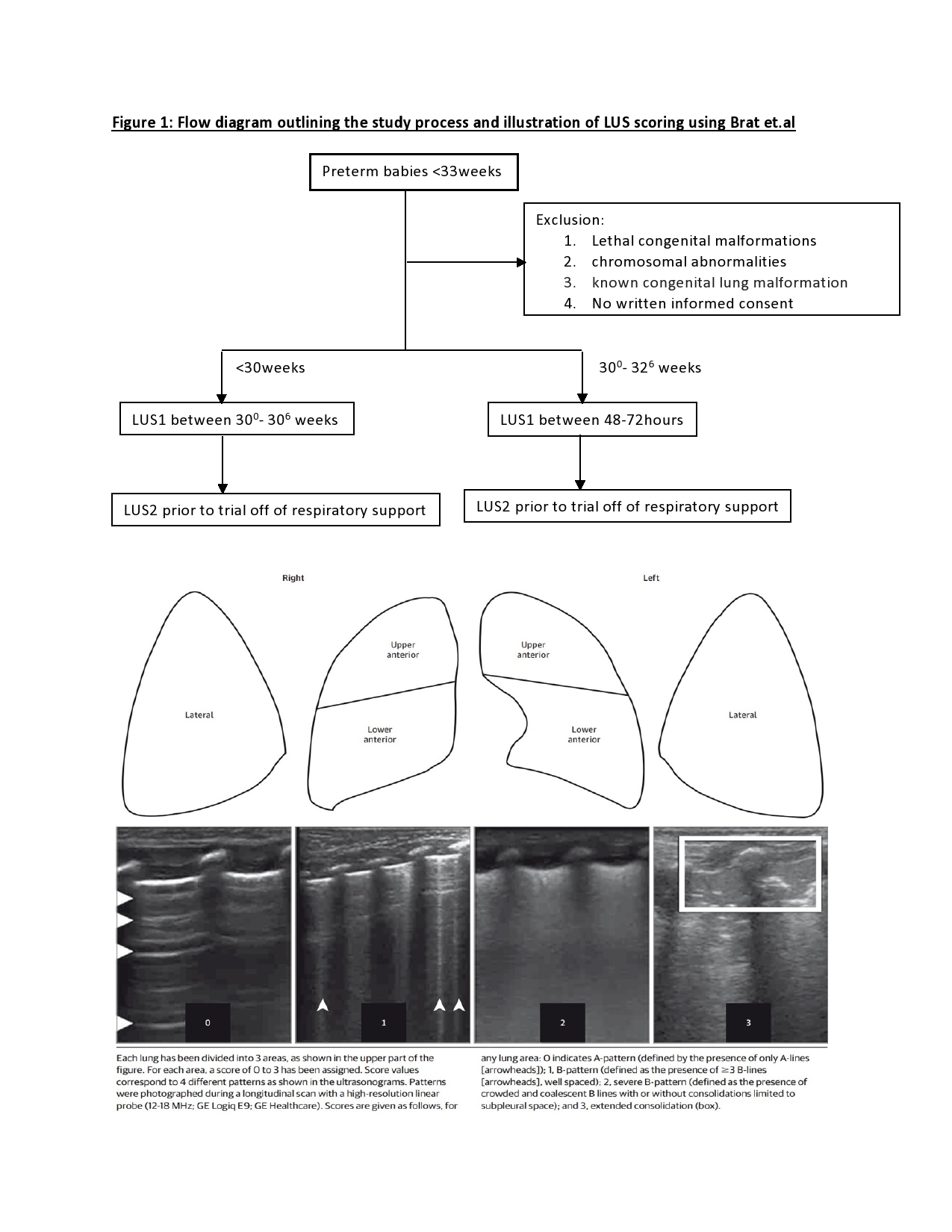
Design/Methods: Prospective cohort study involving preterm neonates born ≤32 weeks needing any respiratory pressure support modes, admitted to a single tertiary care center in Canada between Sept 2022-Sept 2023. Eligible neonates were assessed by LUS at two time points- LUS1 at 30 - 30+6 weeks for those born < 30weeks GA and between 48-72hours of life for those born at 30 - 32+6 weeks GA; LUS2 within 12hours prior to trial off respiratory pressure support to room air or low flow after 32weeks PMA. LUS were scored for disease severity by two independent reviewers using the LUS-sc by Brat et al. (Figure 1). Receiver operator characteristics (ROC) curves analyzed the reliability of LUS-sc to predict the successful cessation of respiratory pressure support to room air or low flow post LUS2.
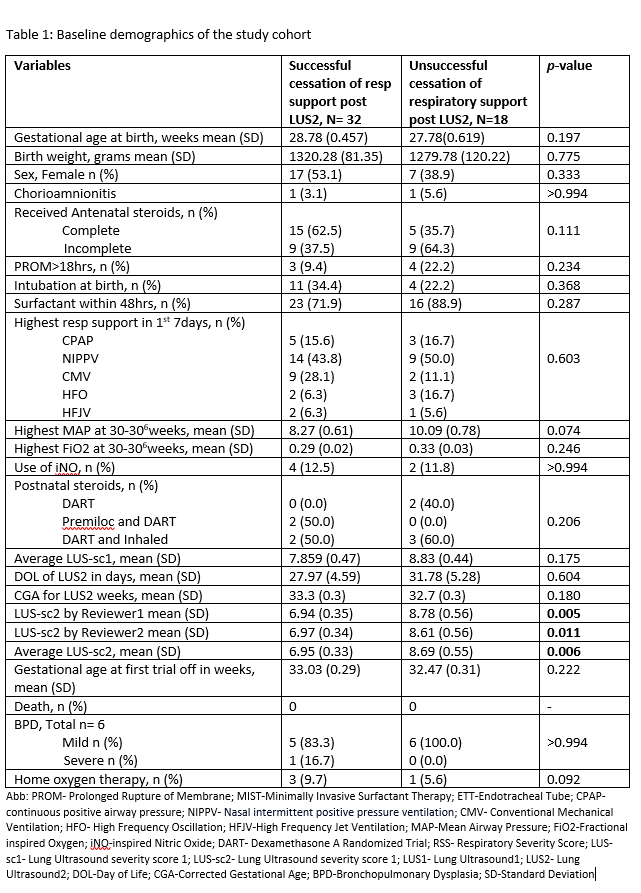
Results: Of 50 preterm neonates included in the study, 32 (64%) were successfully weaned from pressure support after LUS2 at a mean (SD) GA of 33.03 (0.29). The mean (SD) GA at birth was 28.78 (0.46) in the successful group and 27.78 (0.62) in the unsuccessful group (p=0.197). The mean (SD) LUS-sc for LUS2 at which cessation of support was possible was significantly lower from those who failed [6.95(0.33) vs 8.69(0.55), p=0.006] (Table 1). The ROC curve (Figure 2) showed AUC of 0.717 (95%CI=0.56-0.86), for a cut-off of LUS-sc of 7.75, with sensitivity of 0.75 (95%CI=0.60-0.90) and specificity of 0.61 (95%CI=0.38-0.84). Independent of GA at birth and at respiratory pressure support trial off, LUS-sc ≤8 was associated with an increased odd of cessation of support by 9.0 (95%CI=1.9-42.6), p=0.005, and each additional week of GA at first trial off increased the odds of cessation by 2.2 (95%CI=1.1-4.4), p=0.031.
Conclusion(s): LUS is a reliable tool to assess readiness for successful non-invasive respiratory pressure support trial off. A LUS-sc ≤8 was associated with higher successful weaning off of non-invasive pressure support after 32weeks GA.
.png)
