Neonatology
Session: Neonatal Pulmonology - Clinical Science 6: Respiratory/Neuro Outcomes, Steroids
588 - Impact of retinopathy of prematurity (ROP), brain injury, necrotizing enterocolitis (NEC), and sepsis on neurodevelopmental outcomes in preterm infants with bronchopulmonary dysplasia (BPD)
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 588
Publication Number: 588.2938
Publication Number: 588.2938
- VB
Vineet Bhandari, MD DM (he/him/his)
Professor and Division Head
The Children's Regional Hospital at Cooper
Camden, New Jersey, United States
Presenting Author(s)
Background: BPD is associated with adverse long-term outcomes including neurodevelopmental impairment (NDI). ROP, brain injury (severe intraventricular hemorrhage and periventricular leukomalacia), NEC, and sepsis have all been independently associated with poor neurodevelopmental outcomes. BPD often occurs with other co-morbidities like ROP, brain injury, NEC, and sepsis; it is unclear whether and to what extent these conditions contribute to the development of NDI in infants with BPD.
Objective: To examine the contribution of ROP, brain injury, NEC, and sepsis, individually or in combination, on NDI at a corrected age of 18-24 months among infants with BPD.
Design/Methods: Demographics, NICU course, and follow-up data of infants born < 32 weeks gestational age (GA) and with a birth weight (BW) < 1500 grams between January 2010 and December 2020 were collected. The primary outcome measure was NDI at 18-24 months corrected age, defined as blindness, deafness, or a composite score of < 85 on the Bayley Scales of Infant Development (third edition). Chi-square testing was used for pairwise univariate testing. Logistic regression models were used to investigate the relationship between BPD, four neonatal co-morbidities (ROP, brain injury, NEC, and sepsis), and NDI. BPD was defined as the requirement of respiratory support / supplemental oxygen at 36 weeks’ corrected GA.
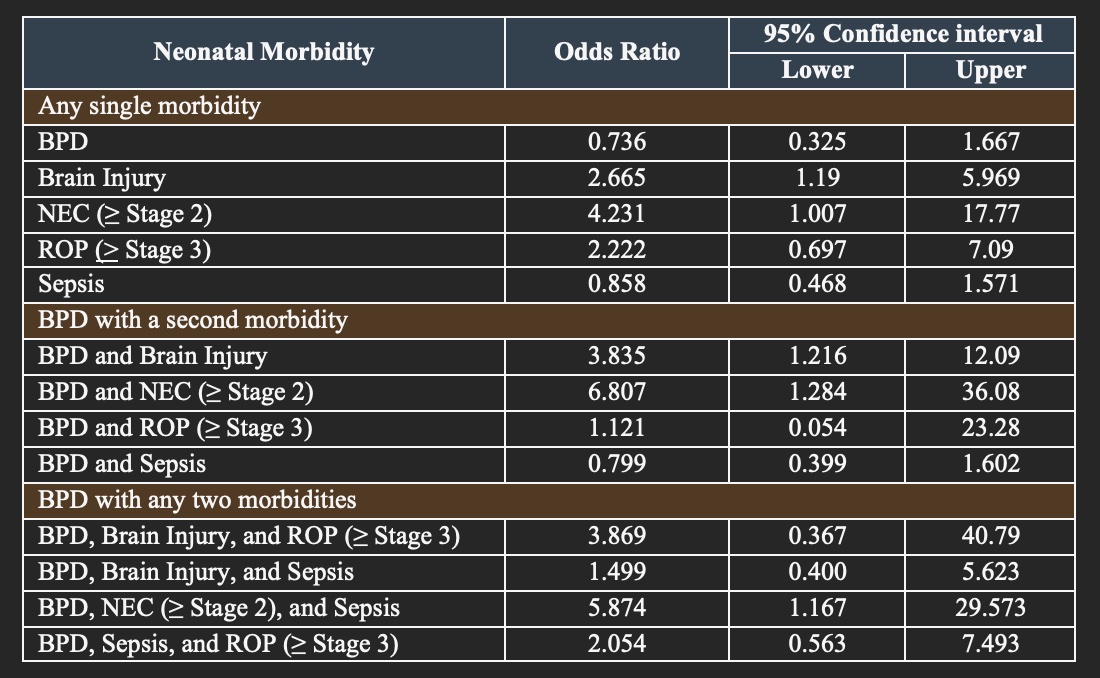
Results: Infants with brain injury, NEC, and ROP had a statistically significant association with the development of NDI at 18-24 months corrected age, whereas BPD and sepsis did not (Table 1). A logistic regression model that adjusted for maternal age, GA, and BW, in addition to the five co-morbidities, determined that infants with brain injury had 2.7 times greater odds of NDI while infants with NEC had 4.2 times greater odds of NDI (Table 2). The combination of BPD and brain injury had 3.8 times greater odds of NDI, while the combination of BPD and NEC had 6.8 times greater odds of NDI (Table 2). The combination of BPD, NEC, and sepsis was the only combination of three co-morbidities that yielded a statistically significant association with NDI. There was no relationship between the number of morbidities and NDI.
Conclusion(s): The results suggest that BPD is not independently associated with NDI in our study cohort. However, infants with BPD had significantly greater odds of NDI if they were also diagnosed with brain injury or NEC. The combination of BPD with two co-morbidities increased the odds of developing NDI.
.jpg)