Neonatology
Session: Neonatal Neurology 6: Clinical
558 - Association of the Timing and Placement of Ventriculoperitoneal Shunt and Gastrostomy Tubes with Meningitis in Infants with Hydrocephalus: A Pilot Study
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 558
Publication Number: 558.1263
Publication Number: 558.1263

Kristin Limpose, MD PhD (she/her/hers)
Residency Trainee
Emory University School of Medicine
Atlanta, Georgia, United States
Presenting Author(s)
Background: Data is lacking to inform the optimal timing and sequence of ventriculoperitoneal shunt (VPS) and gastrostomy tube (GT) placement in neonates with hydrocephalus. Theoretical translocation of gut bacteria through the peritoneal portion of the shunt and seeding of the CNS could increase the risk of meningitis.
Objective: (1) determine the rate of meningitis in infants with a VPS and GT (VPS-GT) compared to VPS alone (VPS), (2) identify meningitis pathogens in infants with VPS-GT versus VPS alone and (3) define the optimal sequence and timing (days) between placement of VPS and GT to minimize risk of meningitis.
Design/Methods: This retrospective cohort study includes infants with VPS placement from two non-delivery tertiary children’s hospital NICUs from January 1, 2010 to August 31, 2022. Children with VPS placed for congenital and acquired causes of hydrocephalus were included. We compared infants with and without GTs, defined as gastrostomy and gastrojejunostomy tubes. The outcome of VPS associated meningitis was defined by positive culture of cerebral spinal fluid after VPS placement. Descriptive statistics will be utilized to answer study objectives.
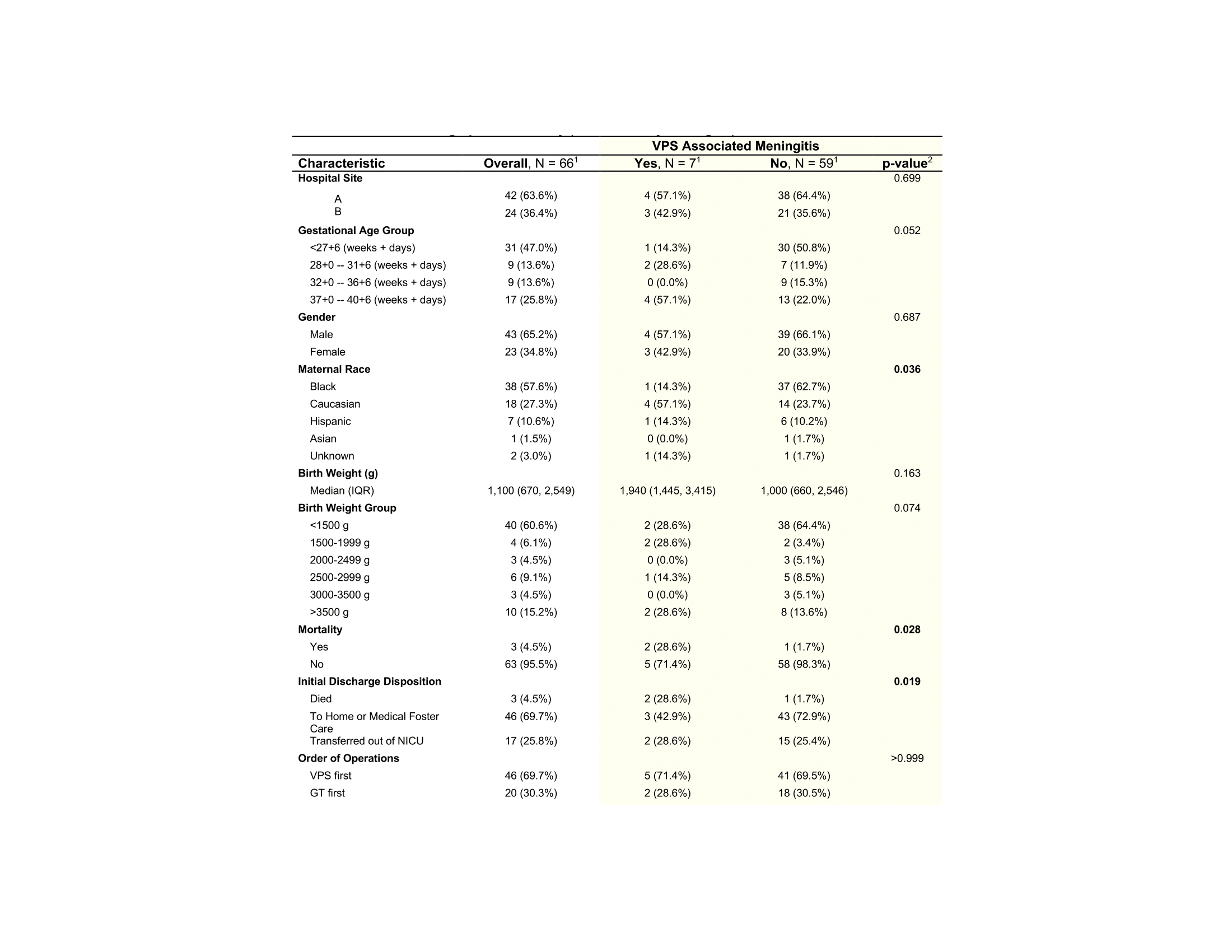
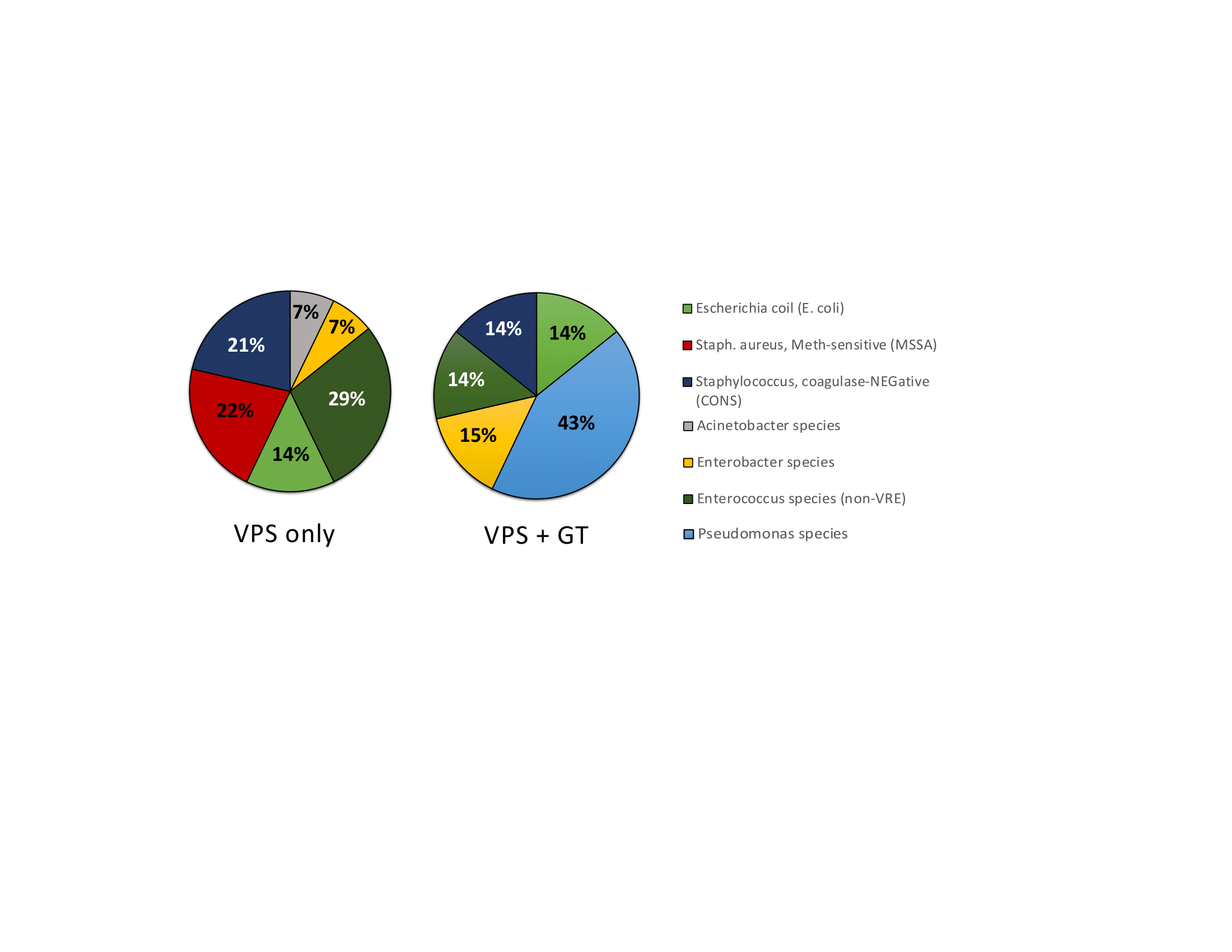
Results: In this cohort of 618 infants with a VPS, 66 (10%) have VPS with GT and 552 (90%) had a VPS only. Demographic and surgical characteristics can be seen in Table 1. The rate of VPS-associated meningitis in VPS-GT infants was 10.6% (95% CI is 4.7%-21.2%), versus 2.6% in VPS infants (95% CI 1.4%-4.3%). Pseudomonas species were the most common etiology of meningitis in VPS-GT infants (43%) while no pseudomonas cases were seen in the VPS infants (Figure 1). Mortality in infants with VPS-associated meningitis in VPS-GT infants was 29% compared to 0% in VPS infants. Of the 7 infants with a VPS and GT who developed meningitis, 71% had a VPS placed before GT and 29% had GT placed before VPS (Table 1). The order of VPS and GT placement did not statistically impact meningitis risk in this pilot study, however a clinical trend towards increased risk of meningitis was observed with VPS prior to GT placement (Figure 2). Time in between procedures was variable, but in those with meningitis a median time between procedures was 48 days. An ROC could not determine the optimal timing between VPS and GT due to small sample size.
Conclusion(s): Meningitis rates are about 4 times higher in infants with a VPS and GT in this pilot study. In contrast to infants with VPS only, pseudomonas was common in VPS-GT infants with meningitis, which may impact mortality and empiric antibiotic regimen. A multicenter study to validate these findings is planned in the near future.
.png)
