Neonatology
Session: Neonatal Fetal Nutrition & Metabolism 3: Enteral Nutrition
442 - Enteral nutritional practices in extremely preterm infants across the United States
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 442
Publication Number: 442.2200
Publication Number: 442.2200

Maria del Mar NMN Romero Lopez, MD, MS (she/her/hers)
Assistant Professor of Pediatrics. Division of Neonatology
UT Health Science Center
Houston, Texas, United States
Presenting Author(s)
Background: There is controversy regarding the most effective enteral nutrition practices for extremely preterm (EP) infants with no widely accepted guidelines.
Objective: The purpose of this study was to provide a comprehensive description of current enteral feeding practices in neonatal units across the US, with the ultimate goal of contributing valuable insights for developing collaborative feeding trials to optimize outcomes in EP infants.
Design/Methods: We conducted a self-administered, IRB-approved, and anonymous online survey using the REDCap database. The survey was distributed to neonatal intensive care staff across the US, through multiple avenues, including the AAP Neonatal and Perinatal Medicine section, the Pediatric Pharmacy Association, The National Pediatric Dietitian Interest Group, and the Pediatrix Medical Group. If we received more than one answer for the center, we only consider the most complete and detailed survey response. Data analysis included descriptive statistics, and we further examined variables, differentiating between academic and non-academic centers, utilizing Pearson's chi-squared test or Fisher's exact test.
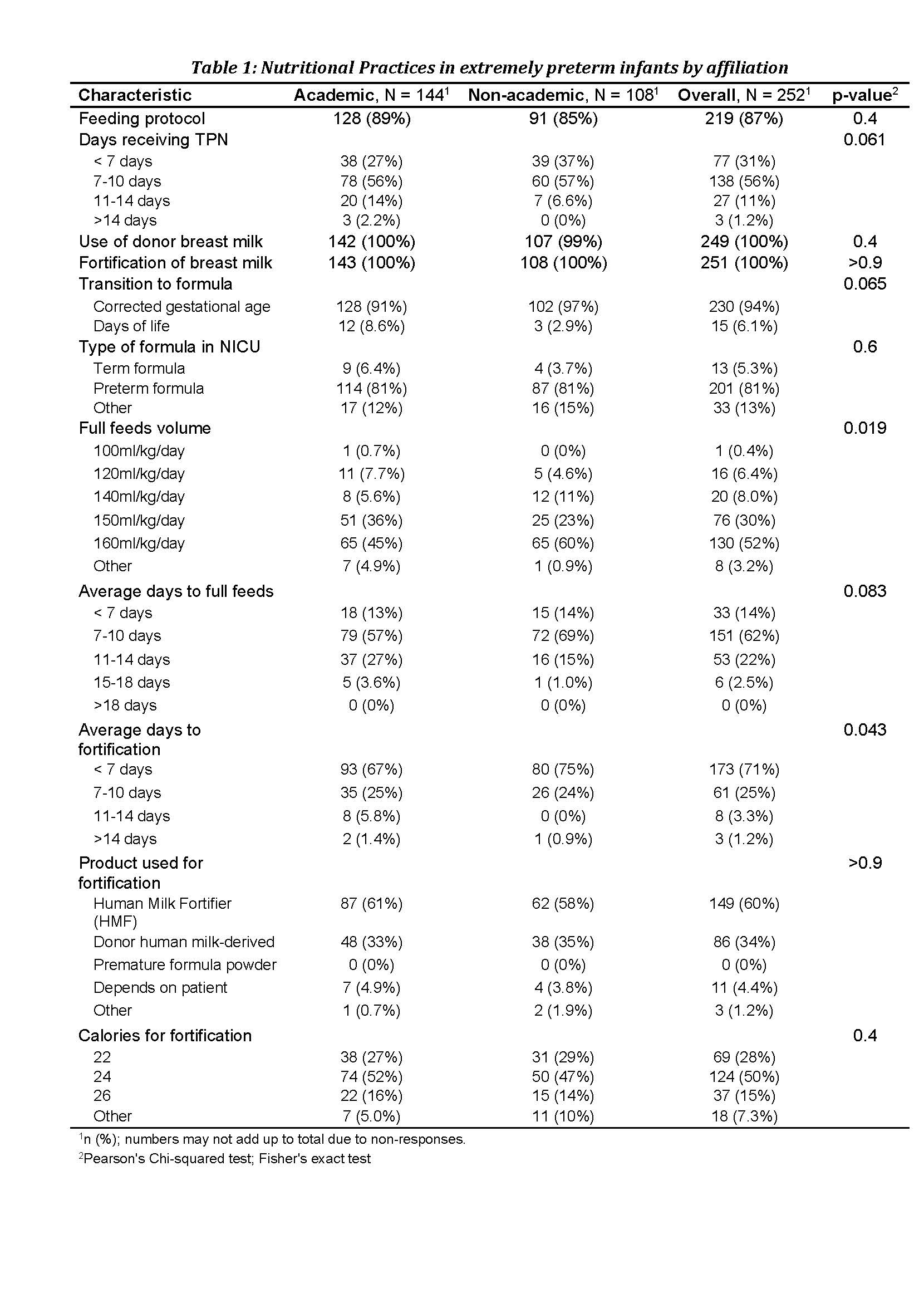
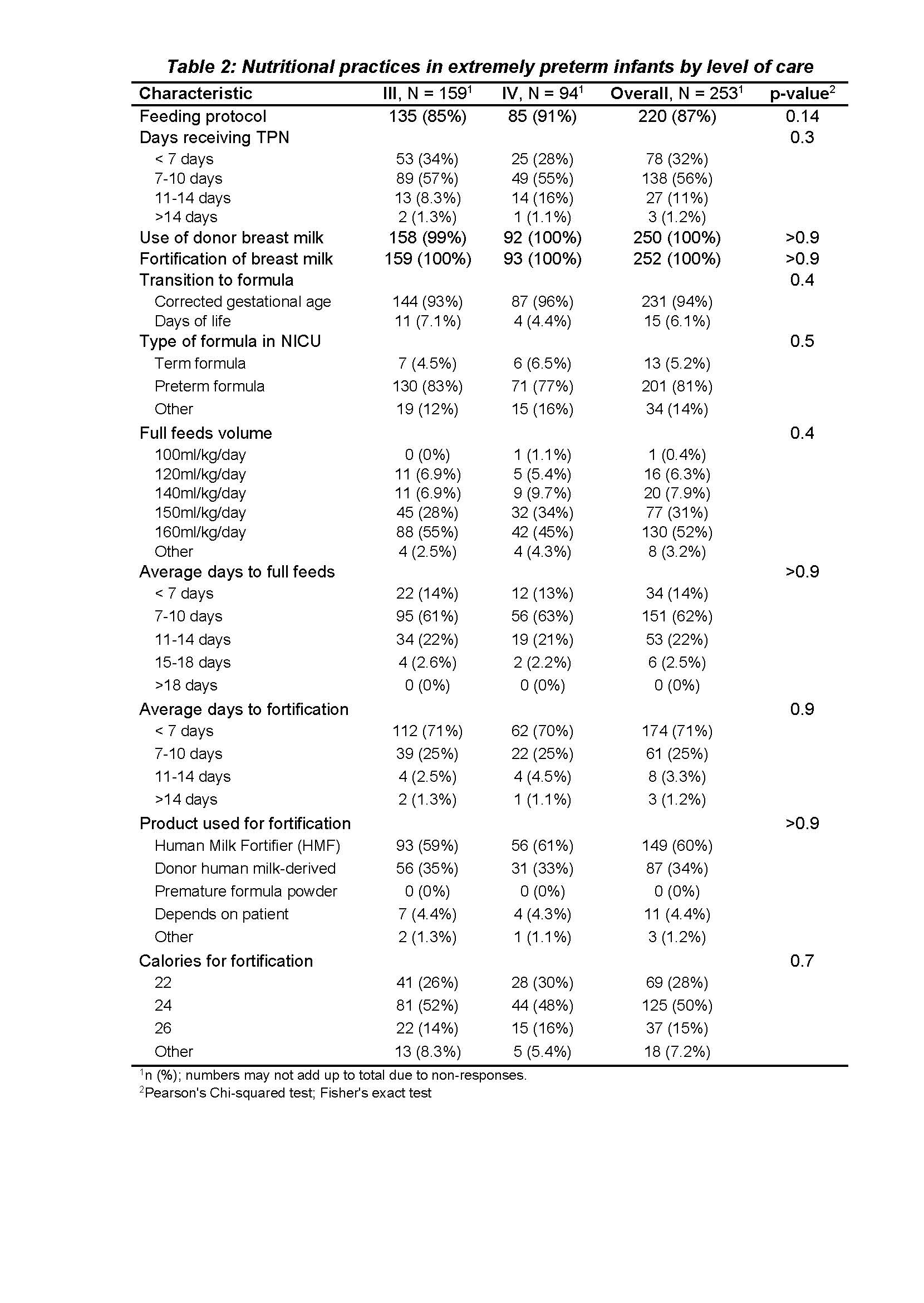
Results: We collected 329 survey responses, with 76 duplicates removed as they represented responses from the same units. The centers were distributed East 17%, Midwest 24%, South 41%, and West 18%. Among responses, 63% were Level III neonatal intensive care units, and 37% were Level IV. Academic centers accounted for 57%. Most units (87%) reported having established feeding protocols, incorporating donor breast milk and fortification into their feeding practices. Over half of the units (52%) defined full feeding as 160 ml/kg/day volume, and 39% defined it as 140 to 150 ml/kg/day. Donor human milk-derived fortification was used in 34% of the centers. No differences in practices between the level of care was identified. However, non-academic centers tended to set higher volume thresholds for full feeding than academic centers (p=0.019), use fortification earlier (p=0.043), and probably advance feeds faster (p=0.083). Approximately 25% of the centers reported that full feeding typically took over ten days.
Conclusion(s): This study highlights variations in the criteria for defining full feeding, the timing of fortification, and the choice of fortification products among different healthcare facilities. These findings underscore the need for further research and collaboration to establish evidence-based guidelines for enteral nutrition in EP infants.