Neonatology
Session: Neonatal GI Physiology & NEC 1: Necrotizing Enterocolitis
513 - A Quality improvement project (QI) to decrease the rate of Necrotizing Enterocolitis.
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 513
Publication Number: 513.2241
Publication Number: 513.2241

sujir nayak, MD
Assistant Professor of Pediatrics
UTSW
Dallas, Texas, United States
Presenting Author(s)
Background: Necrotizing enterocolitis (NEC) is the most common gastrointestinal emergency of very low birth weight (VLBW), preterm infants. Mortality rates approach 40% with survivors often having impaired growth and neurodevelopmental delay. Multiple strategies to decrease the risk of NEC have been described in the literature, such as human milk feeds, standardized feeding protocols, avoidance of agents that reduce gastric acidity, timely removal of central lines and antibiotic stewardship. The frequency of NEC stage ≥ II in VLBW infants at Parkland Health has ranged from 5-9% in 2011-2019, vs 4.5-5.7% in Vermont Oxford Network (VON) NICUs type B.
Objective: To reduce NEC stage ≥ II among VLBW infants and/or ≤ 32 weeks' gestational age (GA) admitted to Parkland NICU by 20% (from 5.5 to 4.5%) from August 2018 to January 2023
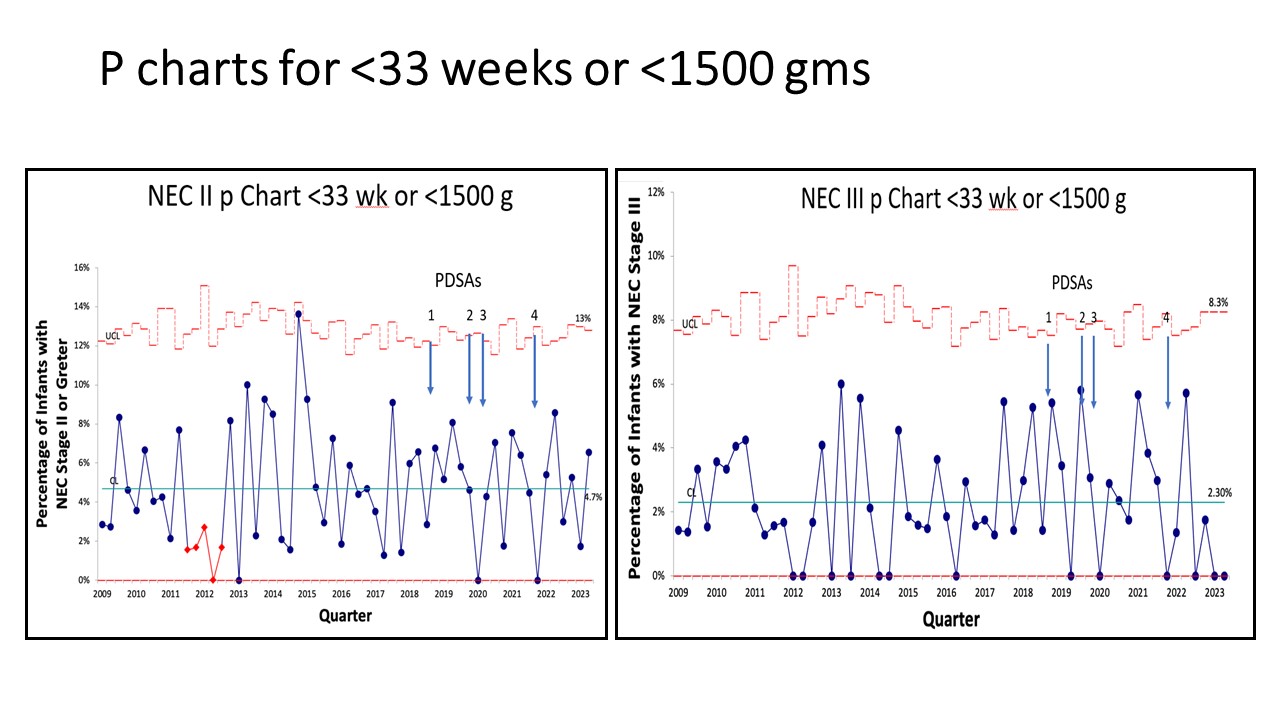
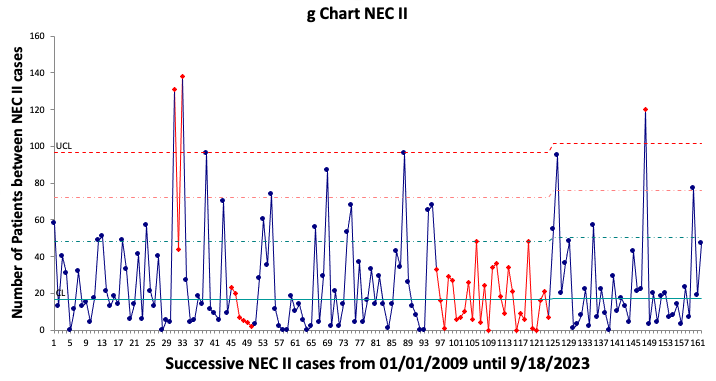
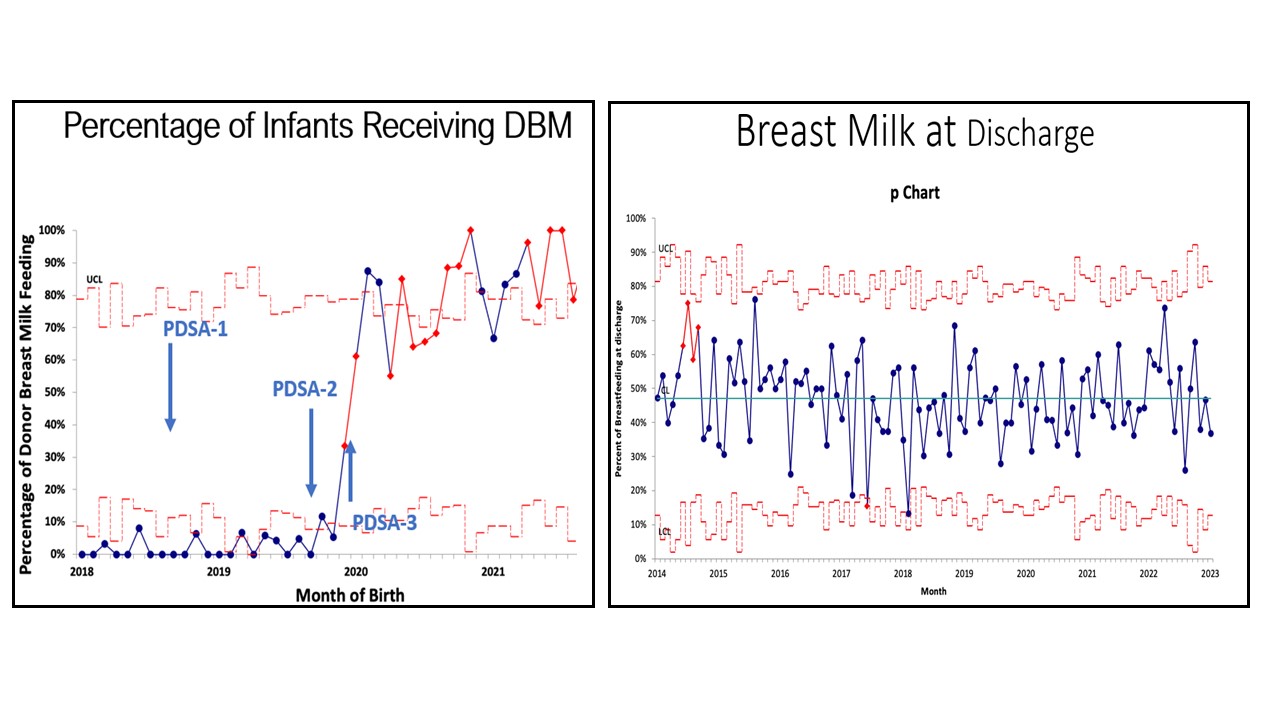
Design/Methods: A key driver diagram was used to find areas to target in our project. The first Plan-Do-Study-Act (PDSA) cycle (PDSA-1) included increasing administration of mother’s own milk (MoM) by education and increasing availability and distribution of pumps before and at delivery. PDSA-2 included encouraging breastmilk pumping as soon as possible and increasing transportation of breastmilk to the NICU. PDSA-3 included administration of donor breastmilk (DBM) with parental consent and pneumatic tubing of MoM. MoM usage after initiation of DBM was used as a balancing measure. PDSA-4 included fresh maternal milk, meeting nutritional requirements for zinc, and delaying initiation of formula until at least 34 weeks postmenstrual age. Since frequent months were observed without NEC especially NEC stage III, Statistical Process Control included p charts and g charts.
Results: The cohort included 1448 neonates and their 1269 mothers. There was no change in frequency of NEC in PDSA-1 and 2. In PDSA-3 there was transient improvement incidence of NEC stage II (p chart) after implementation of DBM. However, the p chart was limited by frequent months with no events. In contrast, sustained improvement in NEC stage II and stage III was observed on g charts after implementation of DBM. There was no decrease in MoM feeding at discharge.
Conclusion(s): This QI project shows sustained improvement in NEC after DBM implementation. It confirms superiority of g charts in assessing NEC compared with p charts.