Asthma
Session: Asthma 1
190 - TEAM Kids: Piloting a Comprehensive Environmental Asthma Care Model
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 190
Publication Number: 190.573
Publication Number: 190.573

Xanthe Gallate, BA (she/her/hers)
Medical Student
Icahn School of Medicine at Mount Sinai
New York, New York, United States
Presenting Author(s)
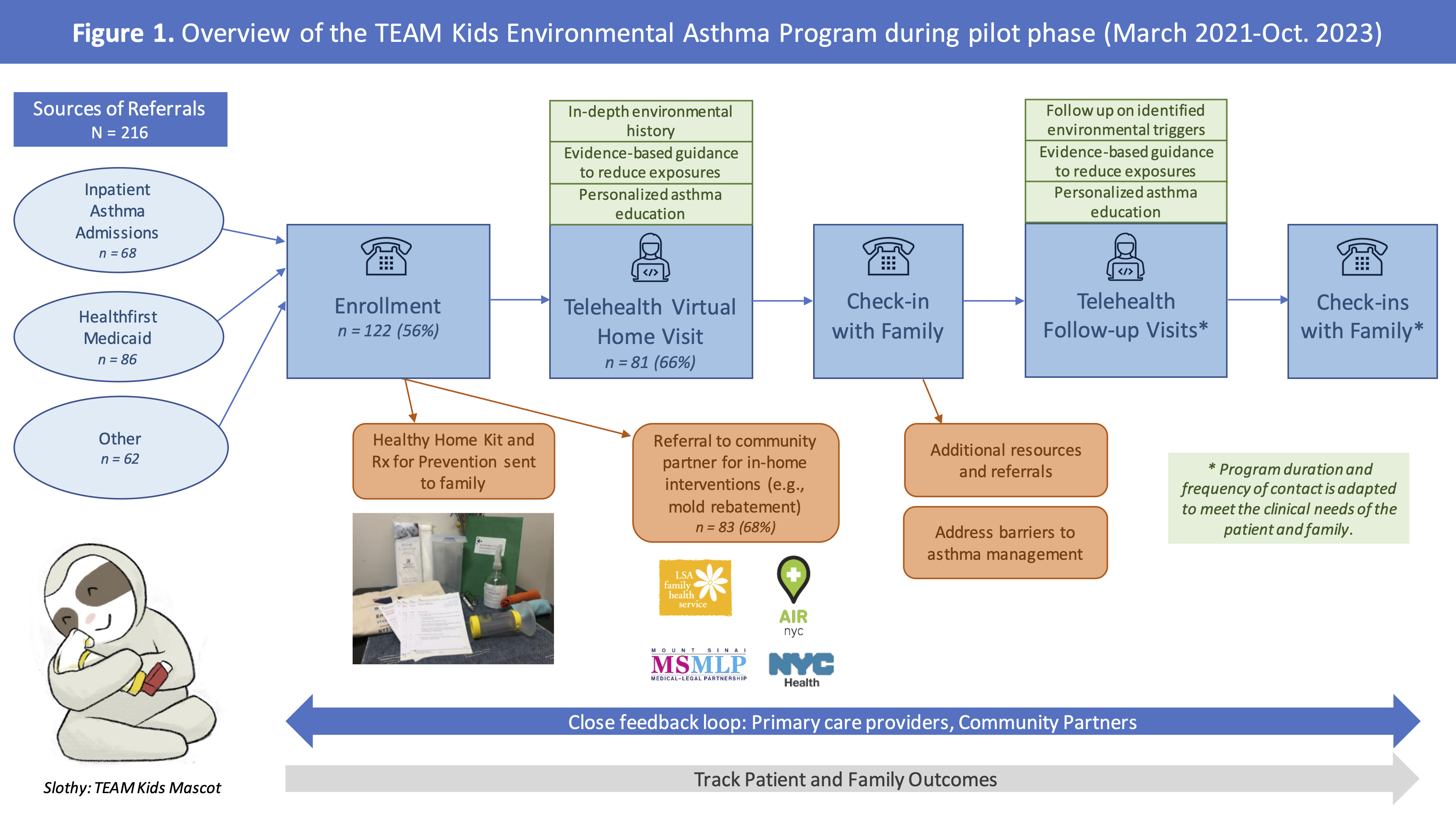
Background: Environmental exposures and unmet social needs impact asthma outcomes, though few pediatric hospitals have clinical programs that comprehensively address these needs. To fill this gap, we developed Team-based Environmental Asthma Management at Mount Sinai (TEAM Kids) to improve outcomes for children with poorly controlled asthma, especially those from communities impacted by structural inequities and asthma disparities.
Objective: Identify environmental and social barriers to optimal asthma management for children participating in the pilot phase of TEAM Kids.
Design/Methods: Patients aged 2-18 years old with poorly controlled asthma were referred to TEAM Kids through Mount Sinai's inpatient pediatric unit, ambulatory clinics, or Healthfirst Medicaid (Fig. 1). Intake/enrollment sessions with families assessed for environmental concerns and barriers to asthma management. Patients were scheduled for their first clinical visit via telehealth within one month of referral. Enrolled families received 2-4 additional visits over 12 months to provide tailored asthma education, evidence-based guidance to reduce asthma-related exposures in their home environment, and referrals to community-based organization (CBO) partners when applicable. For the pilot period, descriptive statistics were performed for enrollment and the first clinical visit.
Results: From March 2021-October 2023, 216 patients were referred and 122 (56%) were reached and successfully enrolled. Of those, 91% had public insurance and 39% lived in public housing (Table 1). Eighty-one percent reported ≥1 common allergen in the home (mold and/or pests) and 64% reported tobacco smoke incursions (Table 2). To address key home environmental asthma triggers, 83 families (68%) accepted a referral to a community-based organization (CBO) partner; 50 of 83 (60%) completed CBO services. Common barriers to asthma management were housing concerns, lack of access to medications, non-adherence to controller medication, and missed doctor appointments. Eighty-one enrolled children (66%) completed their first clinical visit, while 34% were no-shows or unreachable after enrollment.
Conclusion(s): We identified priority impact areas for TEAM Kids, including environmental trigger reduction and medication adherence. Community partners play a vital role in asthma management (e.g., integrated pest management, social supports) and most families completed CBO referrals. Next steps include longitudinal evaluation of asthma outcomes for patients enrolled in TEAM Kids.
.png)
.png)
