Neonatology
Session: Neonatal General 6: POCUS, Technology in NICU
155 - The State of Neonatal Cardiac POCUS - A National Survey
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 155
Publication Number: 155.2255
Publication Number: 155.2255
.jpeg.jpg)
Jack Wren, MD PhD (he/him/his)
Fellow
University of Iowa
Iowa City, Iowa, United States
Presenting Author(s)
Background: Neonatal point-of care ultrasound (POCUS) is an invaluable tool that offers increased accuracy in bedside clinical decision-making and procedures; yet there are little data regarding experience with neonatal cardiac POCUS (cPOCUS). A recent technical report by the American Academy of Pediatrics (AAP) provides some guidance around the use of cPOCUS. Standards, scope of practices, and training requirements around cPOCUS in the neonatal intensive care unit (NICU) are not well defined, especially in relation to neonatal hemodynamics.
Objective: To investigate the current perspectives, training standards, and local governance regarding the use of neonatal cPOCUS.
Design/Methods: cPOCUS was defined by ultrasonography performed at the bedside by practitioners with basic imaging skills as opposed to neonatal hemodynamics where practitioners have completed a formal 1-year fellowship. An online survey was sent to 94 Neonatal Division Chiefs via email with a request to have one anonymous response/program completed by a single knowledgeable representative. The survey was designed to evaluate: (i) presence of cPOCUS and operating procedures, if applicable and (ii) current training and methods of evaluating the completion of training and competency. Descriptive statistics were used.
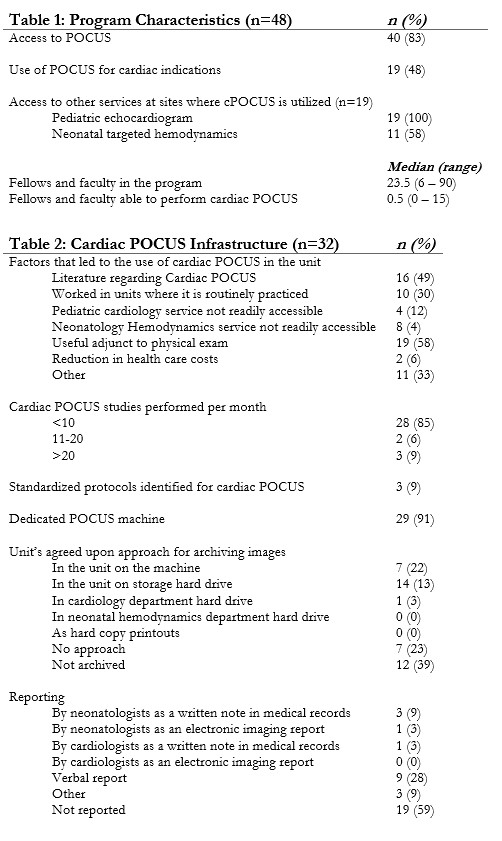
Results: The overall response rate was 51% (48/94). Overall, 40/48 (83%) respondents reported having a POCUS program, of whom 19/40 (47%) responded as performing cPOCUS. Most cPOCUS exams were reported as performed by NICU faculty and fellows. In 85% of the cases, less than 10 cPOCUS studies are performed every month per center. Less than 10% of the programs report utilizing standardized protocols and only 3.2% centers reported archiving studies in a centralized echo-lab server. Standardized documentation is rare with studies either not reported (59.4%) or verbally reported (28.1%). The most common uses for cPOCUS were qualitative assessment of cardiac function, evaluating response to inotropes, central line tip position, or presence of pericardial effusion, and evaluating sudden cardiorespiratory deterioration. Only 9 (22%) programs reported formal cPOCUS training, of whom >50% had no formalized process for assessment of ongoing competency (55.6%) and 2/3 had no final assessment process at the end of the training.
Conclusion(s): Although use of cPOCUS is becoming more common, there is a need for establishing guidelines for infrastructure, training and evaluation of skills. Special emphasis should be placed in determining the scope of practice for appropriate indications.
.jpg)
.jpg)
