Neonatology
Session: Neonatal General 8: ROP, Neurology
308 - Role of genetic susceptibility of intraventricular hemorrhage in very preterm infants: results of a multicenter cohort study
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 308
Publication Number: 308.2920
Publication Number: 308.2920

Xiang Chen, PhD
Shanghai
Children's Hospital of Fudan University
Shanghai, Shanghai, China (People's Republic)
Presenting Author(s)
Background: Intraventricular hemorrhage (IVH) remains a major complication and one of the serious threats to survival for preterm infants and neurodevelopmental outcomes. The early diagnosis of IVH is independently associated with all-cause in-hospital mortality in extremely premature neonates. It is still not clear whether genetic background played a role in IVH in very preterm infants.
Objective: To assess heritable contributions to risk of IVH in a twin cohort restricted to gestational age at birth < 32 weeks.
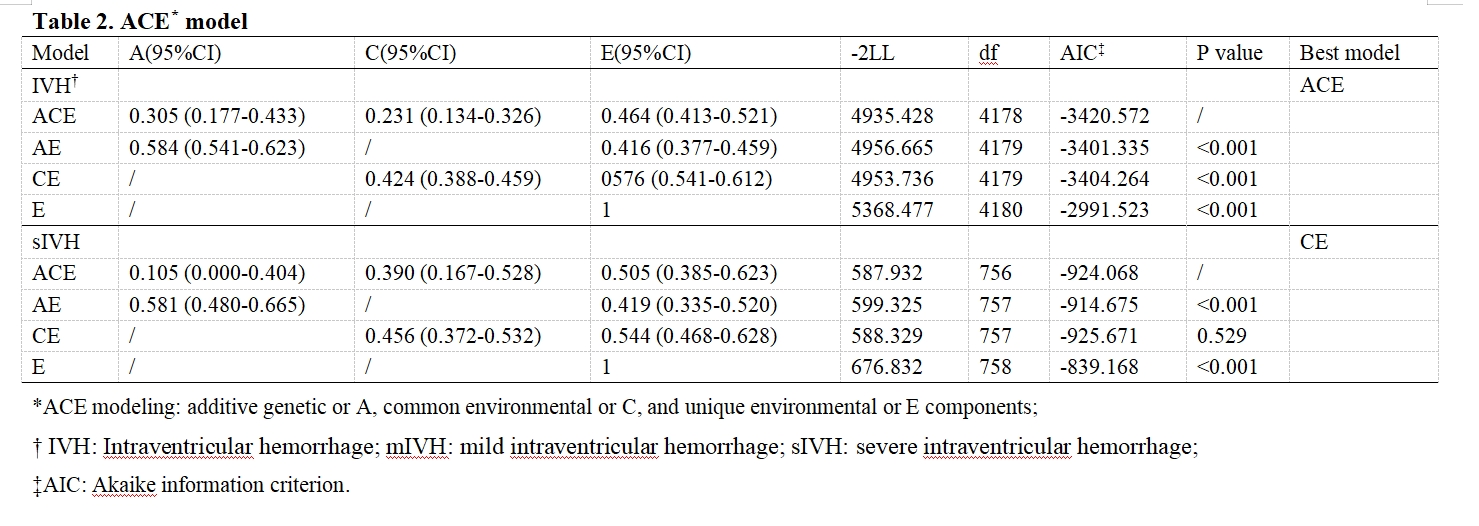
Design/Methods: A total of 2091 twin pairs (1495 dichorionic, 596 monochorionic) with known IVH status who were admitted to member hospitals of Chinese Neonatal Network (CHNN) from January 1, 2019 to December 31, 2021 were enrolled. Three statistical methods applicable to twin cohorts were applied, including Fisher test, intraclass correlations (ICC), and ACE modeling (additive genetic or A, common environmental or C, and unique environmental or E components). Heritability was estimated as percent variability from additive genetic (A). The impacts of clinical characteristics and interventions of IVH or severe IVH (sIVH) were assessed by univariate and multivariable logistic regression modeling.
Results: Both Fisher test (P = 0.002) and ICC analyses (P = 0.005) comparing twin pairs developed IVH revealed significant difference. ACE modeling detected the contribution of heritability to IVH risk (%A = 30.5%, 95% CI [17.7%, 43.3%]) and also environmental factor (%C = 23.1%, 95% CI [13.4%, 32.6%], %E = 46.4%, 95% CI [41.3%, 52.1%]) (Table1-2). By comparing clinical information, no environmental factor was identified. No contribution of heritability was found in sIVH outcome within IVH twin pairs by Fisher and ICC analyses. ACE modeling reported no genetic effect but common environmental (%C = 45.6%, 95% CI [37.2%, 53.2%]) and unique environmental component (%E = 54.4%, 95% CI [46.8%, 62.8%]). After controlling genetic factors, eight clinical factors were detected to be associated with sIVH significantly, including assisted conception, maternal fever, spontaneous preterm birth, lower gestational age, delayed surfactant administration, and higher rates of inotropes , vasoactive medications and sedations.
Conclusion(s): We identified the role of genetic susceptibility of IVH in very preterm infants < 32 weeks gestational age. Quality improvement studies focusing on these potential clinical factors are warranted so as to prevent very preterm infants from progressing to sIVH.
.png)