Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 1: PDA
76 - Comparison of Neurodevelopmental Outcomes of Extremely Preterm Infants Undergoing Surgical Ligation vs. Trans-Catheter Closure of the Patent Ductus Arteriosus
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 76
Publication Number: 76.1830
Publication Number: 76.1830

Dinushan C. Kaluarachchi, MBBS
Associate Professor
University of Wisconsin - Madison
Madison, Wisconsin, United States
Presenting Author(s)
Background: Transcatheter patent ductus arteriosus (PDA) closure has become an increasingly common treatment strategy for preterm infants. Prior studies show an association between surgical ligation and neurodevelopmental impairment. There is a paucity of data on neurodevelopmental outcomes in extremely preterm infants who underwent transcatheter closure versus surgical ligation of the PDA.
Objective: To determine if death or severe neurodevelopmental impairment (NDI) is less frequent in preterm infants treated with transcatheter PDA closure than in those who received surgical ligation.
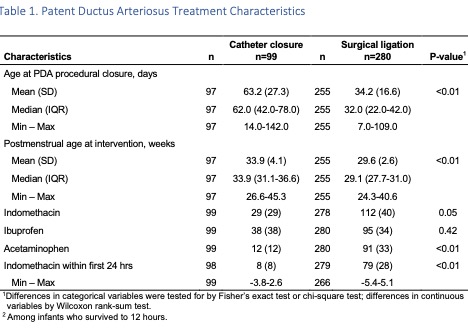
Design/Methods: Retrospective cohort study of infants born at < 27 weeks’ gestation at NICHD NRN sites between 1/1/2016 to 12/31/2019. Infants who underwent surgical PDA ligation were compared to those with transcatheter closure. The primary outcome was death or severe NDI. To assess the relationship between PDA management strategy and outcomes, a 3-level multinomial regression model was developed to estimate propensity scores for the probability of PDA treatment (PDA ligation, catheter closure, medical treatment only) based on demographic and clinical factors. We performed multivariable logistic regression analysis with the outcome of death or severe NDI adjusting for the propensity scores of PDA ligation and transcatheter closure, NRN center, birth year, gestational age and age at procedural closure.
Results: A total of 379 infants who underwent procedural PDA closure were included in the study, 99 infants underwent transcatheter closure and 280 underwent surgical ligation. A third group of 1114 infants who received medical treatment only were included in the multivariable logistic regression analysis. Median gestational age (25.0 vs 24.7 weeks) and birth weight (690 vs 677.5 g) did not differ between the transcatheter closure and surgical ligation groups. Median age at transcatheter closure was significantly greater than age at ligation (62 vs. 32 days, p < 0.01). The primary outcome of death or severe NDI occurred in 49% of infants with transcatheter closure and 39% with surgical ligation (p=0.12). There was no difference in odds of death or severe NDI between transcatheter closure and surgical ligation groups (aOR 0.87 [95% CI: 0.30-2.48]). Both procedural groups had similar odds of death or severe NDI compared to medical treatment only group.
Conclusion(s): Transcatheter PDA closure had similar odds of death or severe NDI compared to surgical ligation. These findings need to be evaluated in large prospective studies as the management practices around transcatheter PDA closure continue evolve.
.jpg)
.jpg)
