Neonatology
Session: Neonatal Pulmonology - Clinical Science 3: Non-Invasive Respiratory Support, RDS
224 - It is Not a Straw: Evaluating the Limits of RAM Cannula
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 224
Publication Number: 224.2741
Publication Number: 224.2741

Andrew Mire, MD, FAAP
NICU Fellow
University of Tennessee Health Science Center College of Medicine
Memphis, Tennessee, United States
Presenting Author(s)
Background: Compared to nasal CPAP, evidence supports Nasal Intermittent Positive Pressure Ventilation (NIPPV) as a noninvasive ventilation method that is associated with lower risk of treatment failure of unsuccessful extubations, air leaks, or mortality. Recently, the RAM cannula has gained popularity as an interface device to provide NIPPV. A concern with RAM cannula when compared to bilevel CPAP for example is that the delivered peak inspiratory pressure (PIP) is lower than the set PIP. Furthermore, as PIP increases, the difference between set and measured PIP widens. As RAM cannula by design requires some leak at the nasal interface, it has been reasoned with supporting evidence that the difference between set and measured PIPs is due to this leak. Another contributing and unstudied factor could be the small internal diameter of the cannula being associated with impeding airflow resistance.
Objective: We hypothesized that as set PIP increases, some drop in measured PIP develops due to airflow resistance in the cannula. In a bench design format, and by using a test lung model, our objective was to evaluate changes in delivered PIP across increasing levels of set PIP when using a RAM cannula to deliver NIPPV.
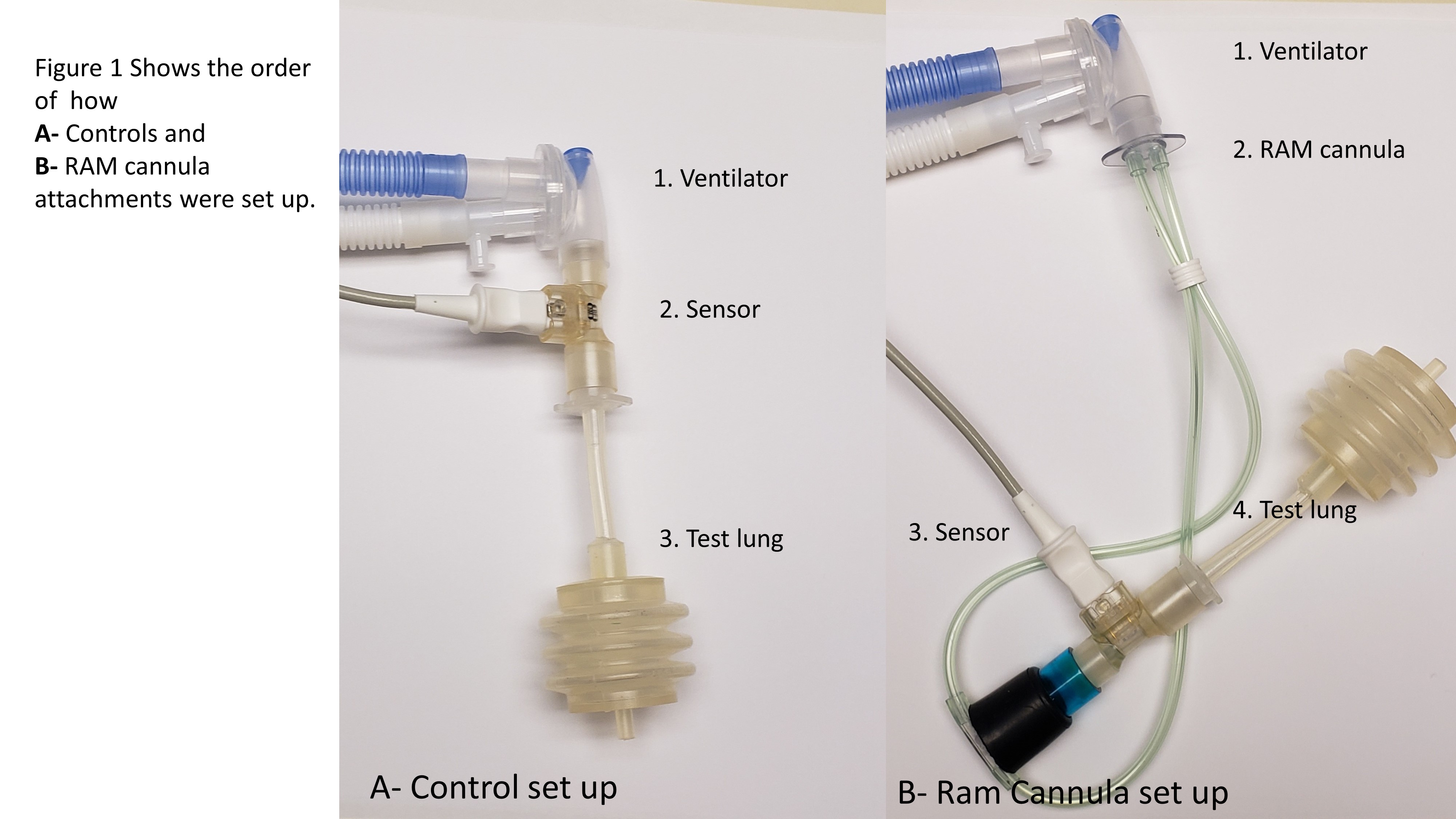
Design/Methods: Methods: A nasal adaptor was designed to which the cannula can be inserted to. The adaptor can then be inserted into the sensor. The system would offer a closed no leak system. A Drager 500 ventilator was used to deliver increasing levels of PIP to a test lung. Other settings were PEEP @5 cm H2O, RR @40, Ti@ 0.5 sec, and slope@0.15 sec. Controls had the following order of attachments: ventilator, sensor, followed by test lung. RAM cannula set up: ventilator, RAM cannula, sensor, test lung, figure1. The N4900 micro-preemie, the smallest, cannula was used. Set and measured ventilator readings were compared.
Results:
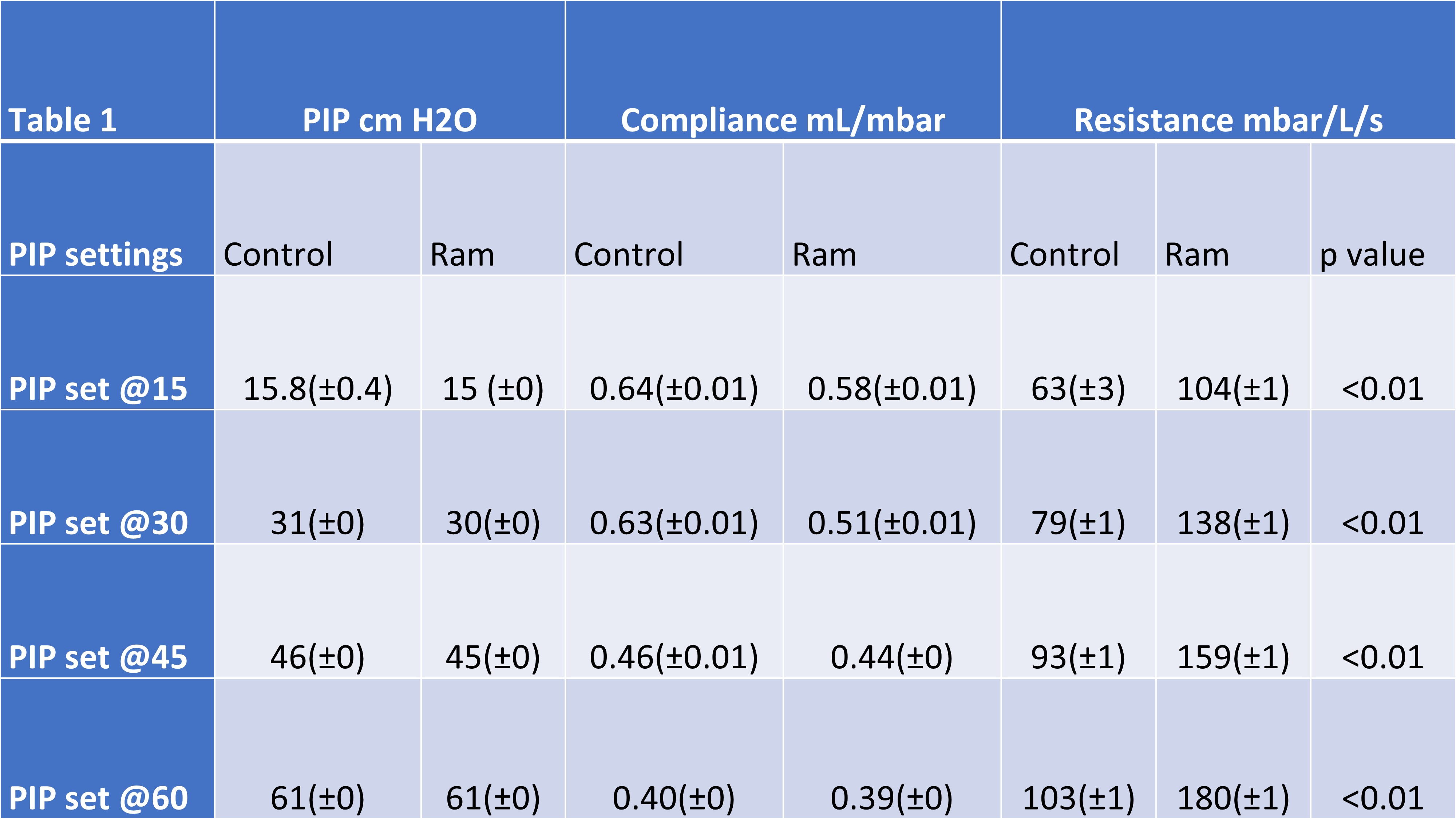
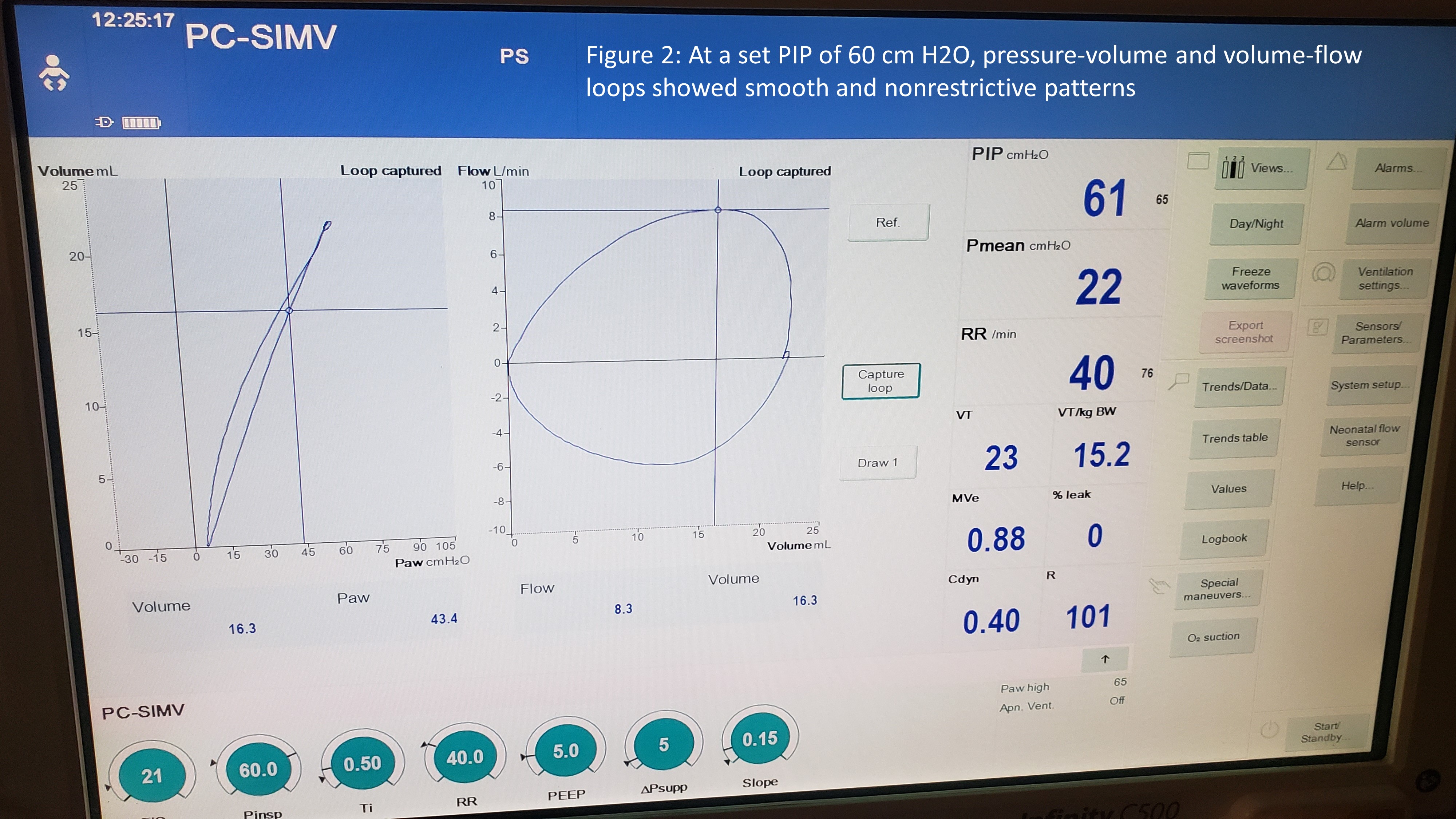
Results: There were not any significant differences between measured PIP levels between control and RAM cannula setups, table 1. As PIP pressure increased, RAM cannula set up maintained target PIP but had significantly higher airway resistance than the control setup. Compliance was comparable. Pressure-volume and volume-flow loops showed smooth and nonrestrictive patterns, figure 2.
Conclusion(s):
Conclusion: When using RAM cannula to deliver NIPPV, any drop in delivered pressure is not due to high airflow resistance from the cannula. This study highlights the importance in using the RAM cannula as designed while maintaining appropriate leak around the nasal interface. At high pressures, tightly fit cannulas are likely to deliver high pressures that may precipitate lung injury.