Neonatology
Session: Neonatal General 4: Nutrition, Feeding, and Growth
105 - Is Provision of Hydrolyzed vs. Intact Bovine Human Milk Fortifier Associated with Clinical Morbidities in Extremely Low Birth Weight Infants?
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 105
Publication Number: 105.620
Publication Number: 105.620

Shannon K. Haines, MD, FAAP (she/her/hers)
Fellow of Neonatal-Perinatal Medicine
University of Nebraska College of Medicine
Papillion, Nebraska, United States
Presenting Author(s)
Background: Adequate nutrition, including appropriate protein provision, has been shown to improve long-term outcomes in extremely low birthweight (ELBW) neonates. As hydrolyzed human milk fortifier (hHMF) is theorized to decrease enteral feeding intolerance in ELBW neonates, a change from non-hydrolyzed HMF (nhHMF) to hHMF was implemented in our level 3 NICU in 2018. Post-transition, clinicians subjectively observed an increased incidence of electrolyte disturbances and worsened clinical outcomes while using hHMF. Specifically, there were concerns that using hydrolyzed protein nutritional products, including hHMF, could lead to increased feeding osmolality which could lead to short- and long-term clinical morbidities.
Objective: This study sought to determine if receiving hHMF is associated with clinical morbidity outcomes in ELBW neonates compared to receiving a nhHMF.
Design/Methods: An IRB-approved retrospective chart review of infants born < 1,000 g (n=47) was completed for infants born in 2016-2019. AKI was defined using the KDIGO criteria and gestational age-specific creatinine cut-off values found to be associated with increased mortality in preterm infants. Type of human milk fortifier received (hHMF vs. NhHMF), Clinical Risk Index for Babies (CRIB II) scores, diagnoses of BPD, ROP, IVH, NEC, and combined enteral + parenteral protein provision (g/kg/day) were collected. Wilcoxon rank sum tests were used to compare continuous variables with dichotomous groups. Fisher’s exact test was used to evaluate categorical variables. Logistic regression was used to model associations of covariates with type of fortifier after adjusting for CRIB II scores. P< 0.05 was considered statistically significant.
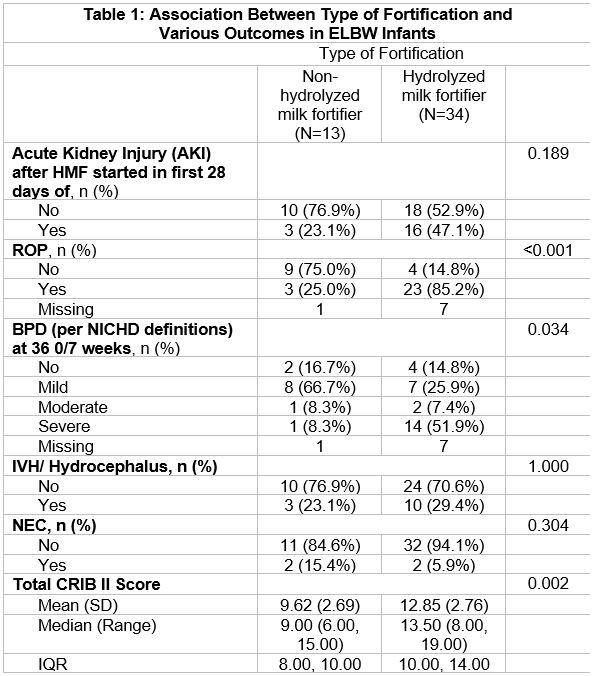
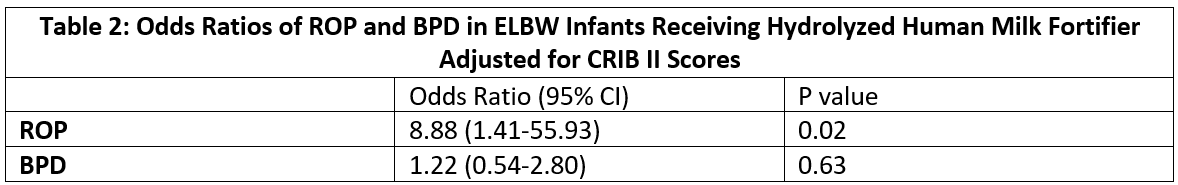
Results: 13 infants (28%) received nhHMF, and 34 infants (72%) received hHMF. There were no significant differences in sex, maternal or infant race or ethnicity, or protein provision between the two groups. Infants receiving hHMF had significantly higher CRIB II scores and rates of ROP and BPD than infants who received nhHMF (Table 1). hHMF was not associated with increased odds of developing NEC or IVH. After adjusting for CRIB II scores, fortification with hHMF was associated with higher odds of developing ROP but not BPD (Table 2).
Conclusion(s): We observed increased odds of developing ROP for infants receiving hHMF, though this could be due to a higher incidence of lower-stage ROP in this population. It was reassuring that there were no increased odds of other comorbidities or poor growth associated with hHMF. Further investigation to evaluate the details of nutrition management could be carried out.