Neonatology
Session: Neonatal Neurology 3: Clinical
45 - Associations between Extracorporeal Membrane Oxygenation and Neuroimaging and Neurodevelopmental Outcomes in Infants with Congenital Diaphragmatic Hernia: A Propensity Score-Matched Analysis
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 45
Publication Number: 45.129
Publication Number: 45.129

Sandy Johng, MD (she/her/hers)
Assistant Professor of Pediatrics
Seattle Children's Hospital
Seattle, Washington, United States
Presenting Author(s)
Background: Infants with congenital diaphragmatic hernia (CDH) are at increased risk of neuroimaging abnormalities and neurodevelopmental impairment. These risks increase if they received treatment with extracorporeal membrane oxygenation (ECMO). It is unknown whether neurologic abnormalities are due to underlying disease severity or exposure to ECMO itself.
Objective: Our objective was to determine whether neuroimaging abnormalities and neurodevelopment impairment can be attributed to ECMO exposure in infants with CDH.
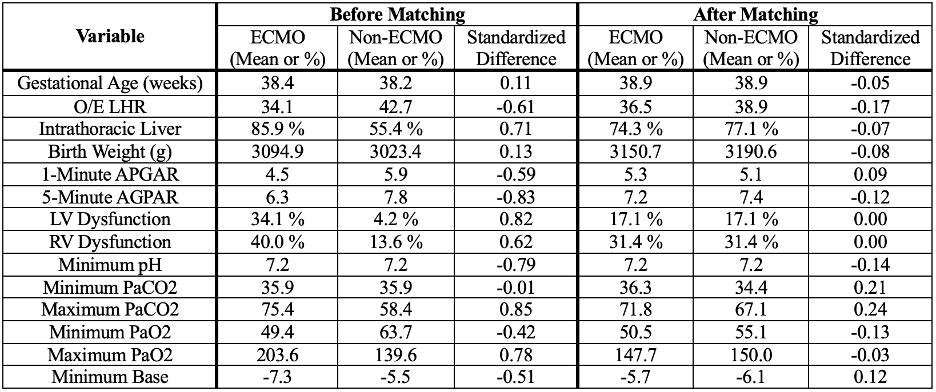
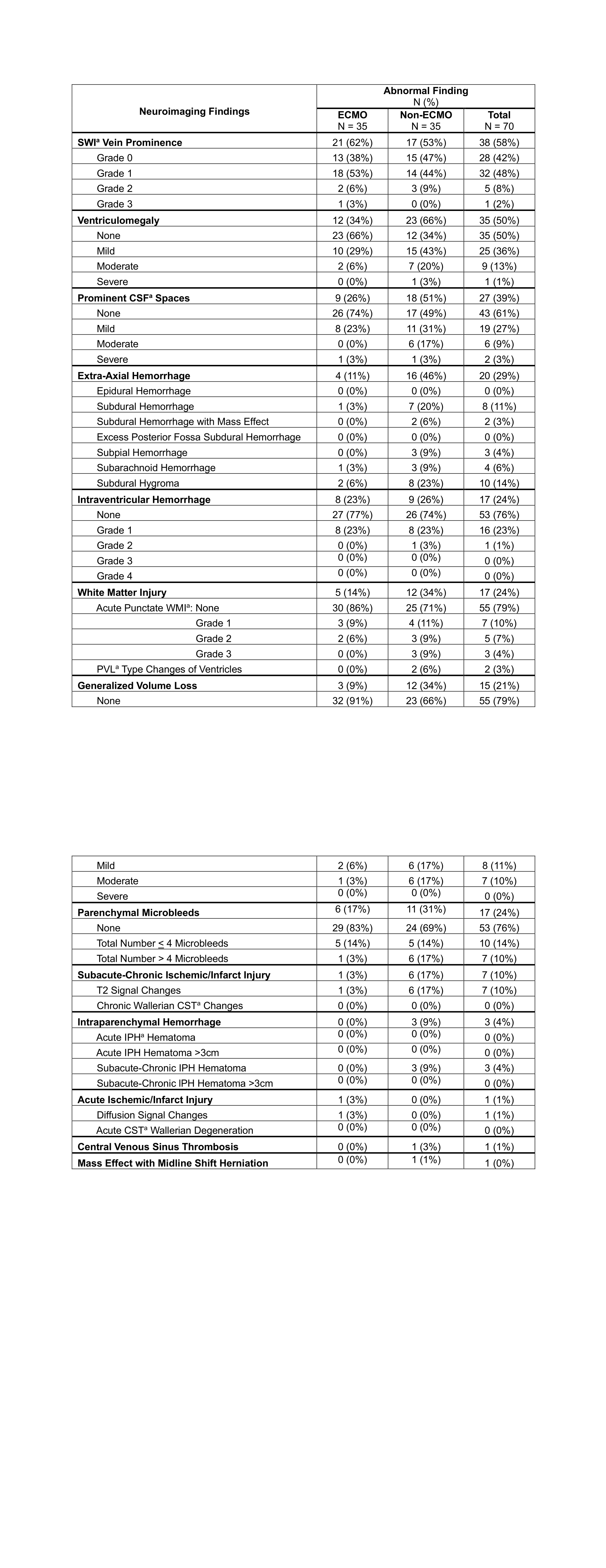
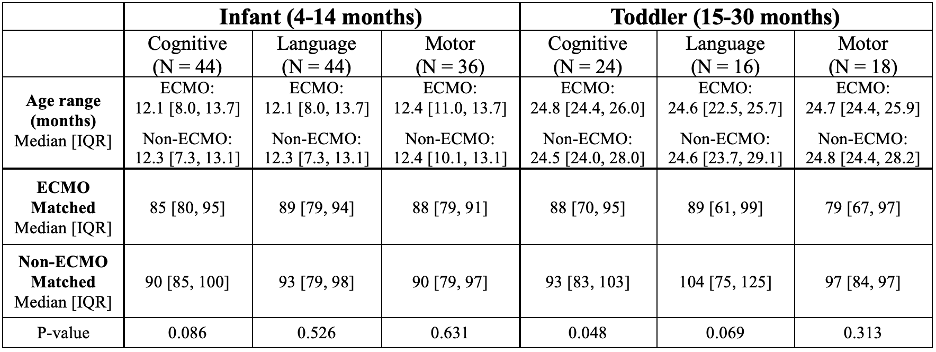
Design/Methods: We conducted a propensity score-matched cohort study using data from a quaternary single-center clinical registry. All patients with CDH born between 2013 and 2021 who underwent active resuscitation at delivery were included for propensity score generation that predicted each infant’s likelihood to receive ECMO treatment. Patients with a diagnostic brain MRI during the birth hospitalization without a chromosomal abnormality that may impact neurologic findings were included in the propensity score match. Brain MRIs were read by a pediatric neuroradiologist who was blinded to clinical data. Development was assessed with Bayley Scales of Infant and Toddler Development, Third or Fourth Edition (Bayley) composite cognitive, language, and motor scores. Bayley data were separated by timing of assessment into infant (4-14 month) and toddler (15-30 month) groups. The relationships between ECMO and neuroimaging as well as neurodevelopment were assessed using Wilcoxon Matched-Pairs Signed-Rank tests.
Results: 70 infants (35 pairs) met eligibility criteria for the propensity score-matched analysis. Balance after propensity-score matching is shown in Table 1. Neuroimaging findings stratified by ECMO exposure are presented in Table 2. Significantly more neuroimaging abnormalities were found in ECMO-matched compared with non-ECMO-matched patients (p-value < 0.001). Out of 66 survivors, 36-44 (55-67%) infants and 16-24 (24-36%) toddlers had Bayley testing. In the toddler group, the ECMO-matched patients had significantly worse cognitive (p-value 0.048) and marginally worse language (p-value 0.069) scores compared with the non-ECMO-matched patients (Table 3).
Conclusion(s): In patients with a similar probability of receiving treatment with ECMO, removing ECMO treatment significantly decreases neuroimaging abnormalities, and may be associated with improved 15-30 month cognitive and language scores. One area of future research is to investigate potentially modifiable aspects of ECMO treatment that may be optimized to improve neurologic outcomes.