Asthma
Session: Asthma 2
207 - Multi-disciplinary Asthma Education Initiative
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 207
Publication Number: 207.188
Publication Number: 207.188

Poonam Vasant Nayak, MD (she/her/hers)
Resident
Children's Hospital of New Jersey at Newark Beth Israel Medical Center
Newark, New Jersey, United States
Presenting Author(s)
Background: Asthma-related morbidity and mortality for children in Newark are disproportionately higher than the norm, due to the substantial disparities in social & health determinants and in healthcare experienced by them. One in four children in Newark has asthma1. The hospitalization rate is 150 percent greater for children living in Newark than in the rest of New Jersey, and more than thirty times the nationwide rate². Although asthma-related deaths are rare in children, Newark experienced an average of one death a year from 2010 to 2017, according to the New Jersey Department of Health³
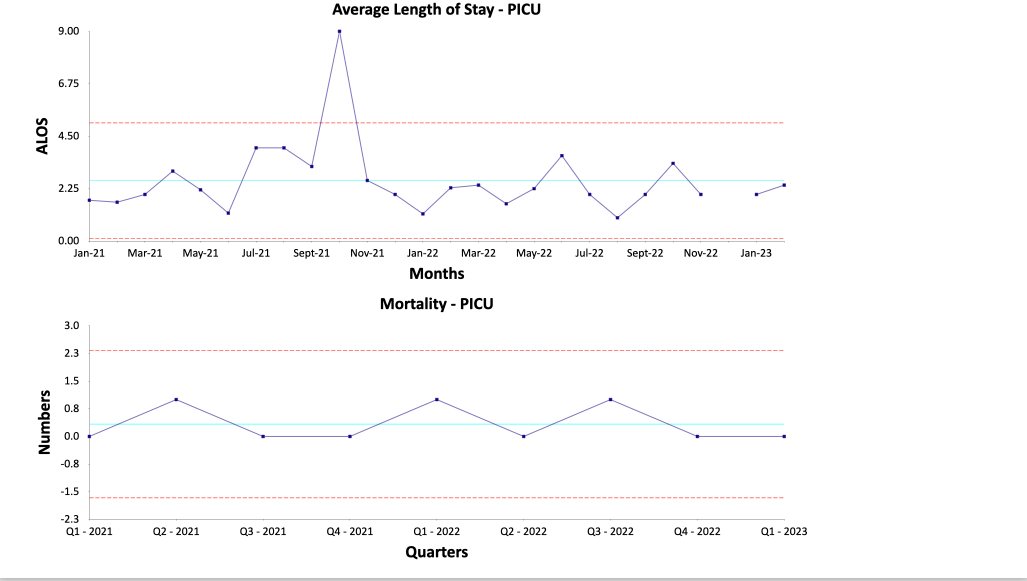
Objective: To reduce the asthma related mortality in pediatric patients from 2 in 2021 to 0 by end of 2023 via multi-disciplinary bundled education and service to the patients admitted for Asthma to Inpatient Pediatrics (IP) and Pediatric Intensive Care Unit (PICU) at CHoNJ.
To reduce length of stay in PICU patients by 20% by end of 2022 by switching from continuous albuterol nebulization directly to MDI treatment
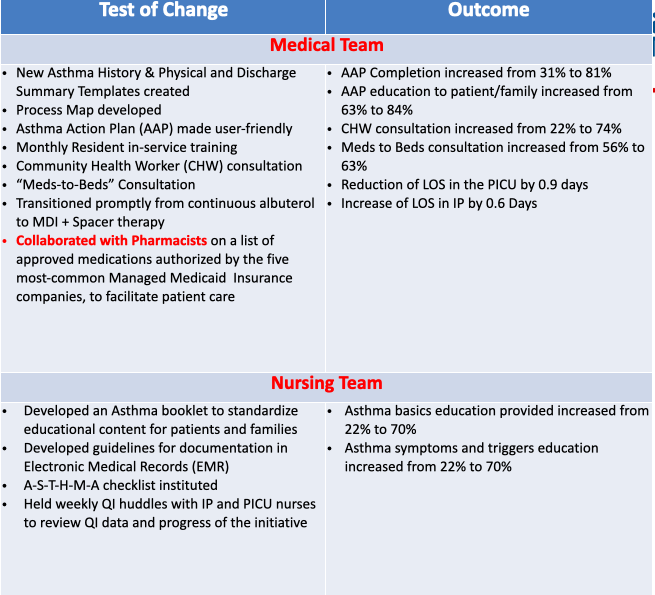
Design/Methods: An inter-disciplinary group was formed, composed of Physicians, Nurses, Respiratory Therapists (RTs), a Community Health Worker (CHW), a “Meds to Beds” professional, and a Pharmacist.
A pre-implementation survey, conducted for all team members to evaluate their level of comfort with teaching asthma-related content to patients and families, revealed low levels of confidence and significant person-to-person variation.
A multi-faceted approach with physicians, nurses, and RTs was used for educating patients and their families.
Baseline data was collected from October 2021 through March 2023.
Bundled services — asthma education / meds-to-beds service / CHW consultation — were provided.
Results: Comprehensive asthma education was provided to 75% of patients and families
All elements of bundled services were provided to 72% of patients
There were no re-admissions for asthma (during the 30-day period after discharge) nor any asthma-related deaths during the study period.
Length of Stay (LOS) in PICU reduced by 0.9 days with a concomitant increase in LOS by 0.6 days in IP
The interventions resulted in a net decrease of ~$72K in the cost of hospitalization of our asthmatics.
Conclusion(s): The reduction in LOS in PICU resulted from an earlier transition from continuous albuterol to MDI than had been the practice before, and led to a faster transition to IP service, with the resultant increase in LOS in IP.
The decreased hospitalization costs provide a strong additional justification for the establishment of a comprehensive multi-disciplinary team to care for children with asthma in Newark, NJ.