Developmental and Behavioral Pediatrics
Session: Developmental and Behavioral Pediatrics 4: Potpourri
600 - Parent-Clinician Miscommunication after Pediatric Developmental Screening
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 600
Publication Number: 600.2062
Publication Number: 600.2062

Lindsay Schlichte, MS (she/her/hers)
Medical Student
Duke University School of Medicine
Garden City, New York, United States
Presenting Author(s)
Background: Effective parent-clinician communication during well-child check (WCC) visits supports parental understanding of developmental concerns and plans for referrals or early intervention services. Miscommunication may be a barrier to this process, hindering parents' ability to navigate or access referral services.
Objective: (1) Investigate discrepancies between post-WCC data gathered from both clinicians and parents surrounding developmental concerns and referrals. (2) Identify factors associated with discrepancies.
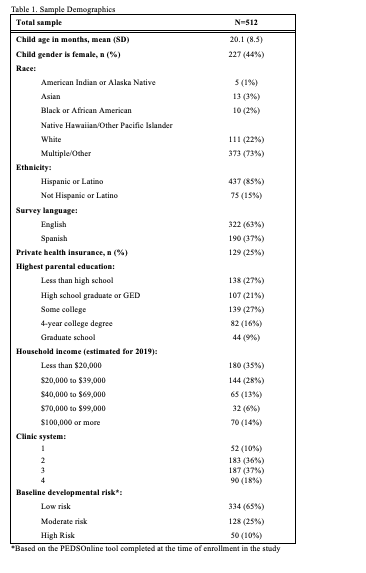
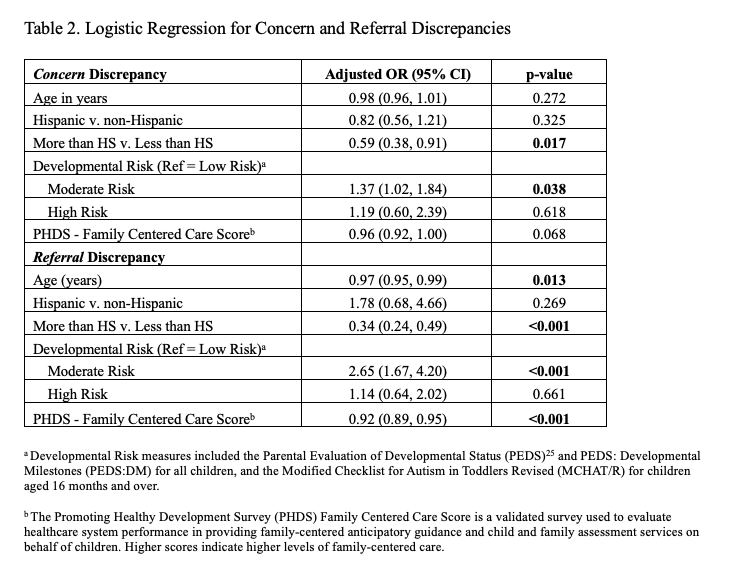
Design/Methods: We conducted a secondary analysis of data from the Achieving My Potential (AMP) study, a randomized controlled trial assessing a telephone-based childhood developmental care coordination system. English and Spanish-speaking families with children aged 12-42 months were recruited from community clinics. Data included baseline demographic and developmental assessment results, parental post-WCC surveys, and medical record data (chart abstraction) regarding the presence of a developmental concern and referrals for services. Two discrepancy types were defined based on data from parent surveys and chart abstractions: (a) concern discrepancies: differences in parent report versus chart documentation of discussing developmental concerns; (b) referral discrepancies: differences in parent report versus chart documentation of referral for evaluation or services. Discrepancy frequencies were calculated and logistic regressions examined characteristics associated with concern and referral discrepancies.
Results: Among 512 enrolled families, there were 94 (18%) concern discrepancies, of which 73 (78%) parents reported discussing a concern when the medical record did not. There were 43 (8%) referral discrepancies, of which 27 (63%) had a referral indicated in the chart but not by parent report. Children at moderate risk for developmental delay had greater odds of concern discrepancy (AOR 1.37; p < 0.05) and a referral discrepancy (AOR 2.65; p < 0.001). Having parents with at least a high school education was associated with lower odds of concern discrepancy (AOR 0.59; p < 0.05) and referral discrepancy (AOR 0.34, p < 0.001). Older parental age (AOR 0.97; p < 0.05) and higher family-centered care scores (AOR 0.92; p < 0.001) were also associated with lower odds of a referral discrepancy.
Conclusion(s): Miscommunication during WCCs may impact families' understanding of next steps and access to early intervention services. Clinicians might take extra care to ensure common understanding for families at greater risk for miscommunication.