Neonatology
Session: Neonatal Pulmonology - Clinical Science 2: Lung Imaging, Lung Function
208 - Comparison of oxygen saturation and work of breathing indices in preterm infants with and without bronchopulmonary dysplasia at discharge
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 208
Publication Number: 208.2967
Publication Number: 208.2967
- KK
Kelley Kovatis, MD (she/her/hers)
Attending Physician
ChristianaCare
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Thoracoabdominal asynchrony (TAA) is commonly seen in preterm infants secondary to highly compliant rib cage and poor compensation by immature respiratory muscles. Respiratory inductive plethysmography (RIP) is a noninvasive way to objectively assess work of breathing (WOB) indices. Premature infants with respiratory distress have reported TAA but the persistent impact of bronchopulmonary dysplasia (BPD) on TAA at discharge has not been established.
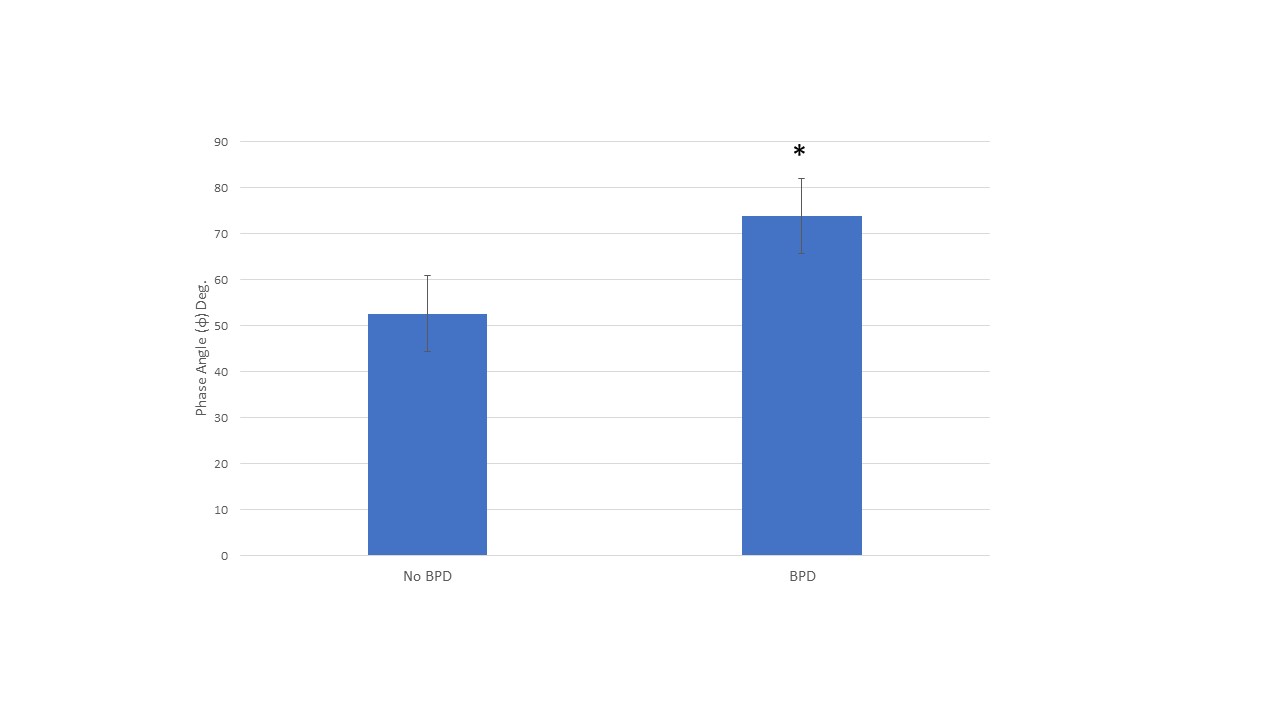
Objective: To compare WOB indices [phase angle(Փ), labor breathing index (LBI), RR, HR] in premature infants with a diagnosis of BPD to premature infants without a diagnosis of BPD in the supine position at the time of discharge. We hypothesized WOB indices in patients with BPD would be greater than in patients without BPD.
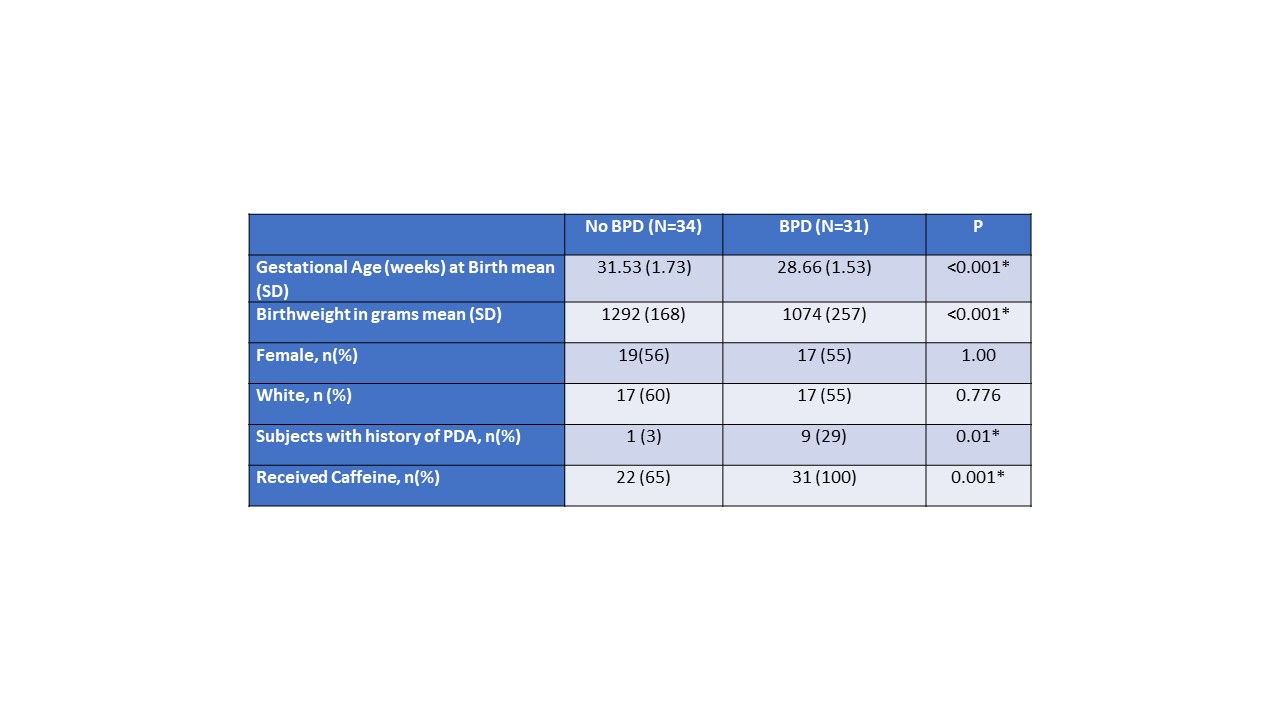
Design/Methods: This is a prospective observational study of infants born with a birth weight of < 1500g and at >26 completed weeks’ gestation at a single center NICU. RIP and pulse oximetry measurements (mean ± SEM) were made in the supine position within 7 days of discharge. PneuRIP, a portable, bedside software was used to provide real time clinical data. Diagnosis of BPD was based on the 2018 NICHD criteria.
Results: This study included 31 infants diagnosed with BPD and 34 infants without BPD. Infants diagnosed with BPD were chronologically older (p < 0.001) and had an older post menstrual age (p < 0.001) at the time of discharge compared to infants without a diagnosis of BPD (Table 1). Infants diagnosed with BPD had increased phase angle [BPD Φ=73.90 (8.2) vs NoBPD Φ=52.60 (8.2), p=0.039] (Figure 1). Infants diagnosed with BPD had decreased saturations [BPD SpO2=96% (0.4) vs NoBPD Sp02 98% (0.3), p= < 0.001], increased time with saturations less than 85% [BPD %=2.74 (0.7) vs NoBPD %=0.91 (0.4), p=.018], and increased time with saturations less than 80% [BPD %=1.57 (0.5) vs NoBPD %= .52 (0.3), p=0.045] (Table 2). There was no difference in heart rate or breaths per minute for infants with BPD versus controls. No difference in phase angle and severity of BPD.
Conclusion(s): Premature infants with BPD demonstrated increased TAA and had lower saturations compared to infants without BPD at discharge despite being chronologically older and being discharged at an older corrected gestational age. The impact of BPD on breathing patterns persists at discharge and suggests these patients may have residual lung and/or respiratory muscle dysfunction.
.jpg)