Neonatology
Session: Neonatal Neurology 4: Clinical
529 - The use of a novel multimodality monitoring approach to evaluate critically ill neonates
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 529
Publication Number: 529.1177
Publication Number: 529.1177

Gabriel F. T Variane, Gabriel Variane, MD, PhD (he/him/his)
Neuro-NICU Medical Director
Santa Casa de São Paulo
São Paulo, Sao Paulo, Brazil
Presenting Author(s)
Background: Multimodality monitoring facilitates the diagnosis and prevention of neurological injury in the setting of hemodynamic compromise in critically ill patients. A multimodal monitoring approach may aid in identifying the hemodynamic changes and the risk of cerebral injury by simultaneous, time-synchronized presentation of datastreams from near-infrared spectroscopy (NIRS), amplitude-integrated electroencephalography (aEEG) and other vital signs.
Objective: Demonstrate how comprehensive multimodal monitoring provided rapid recognition of the hemodynamic status and informed treatment decisions.
Design/Methods: We describe 3 cases of multimodal monitoring including aEEG, NIRS, and other vital signs in high-risk infants.
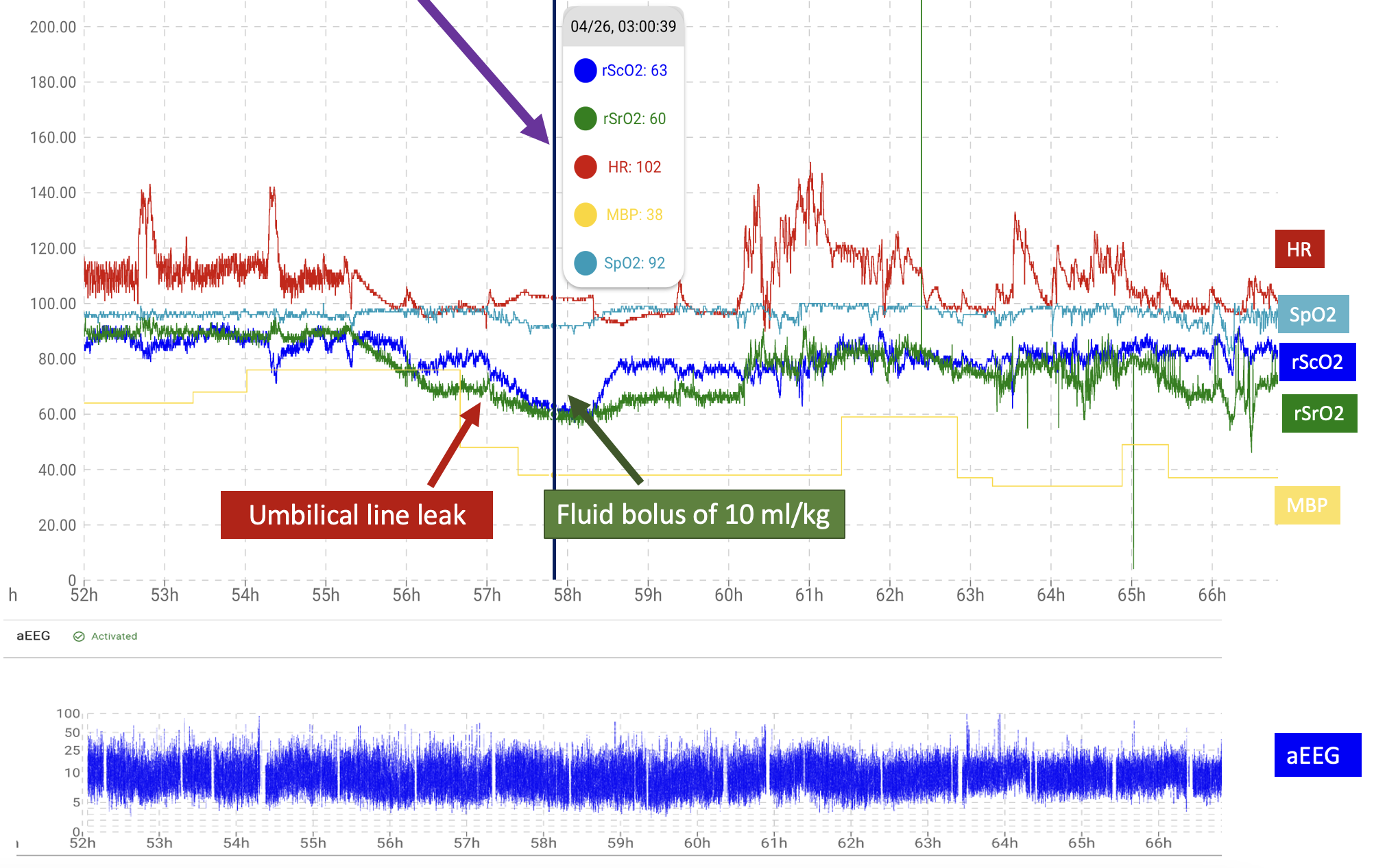
Results: Case 1: A preterm with gestational age (GA) 30 weeks, birthweight (BW) 1020g, was admitted to the NICU with respiratory distress and was stable on CPAP with FiO2 21%. During the 3rd day of life (DOL) he had a decrease in cerebral saturation (rScO2) from ~85% to 63% and renal saturation (rSrO2) from ~90% to 60%. A clear reduction in heart rate (HR) variability was also noticed. A clinical exam was performed and an umbilical catheter leak was noted prompting insertion of a new central line. After a fluid bolus of 10ml/kg recovery of both rScO2 and rSrO2 was seen (Figure 1).
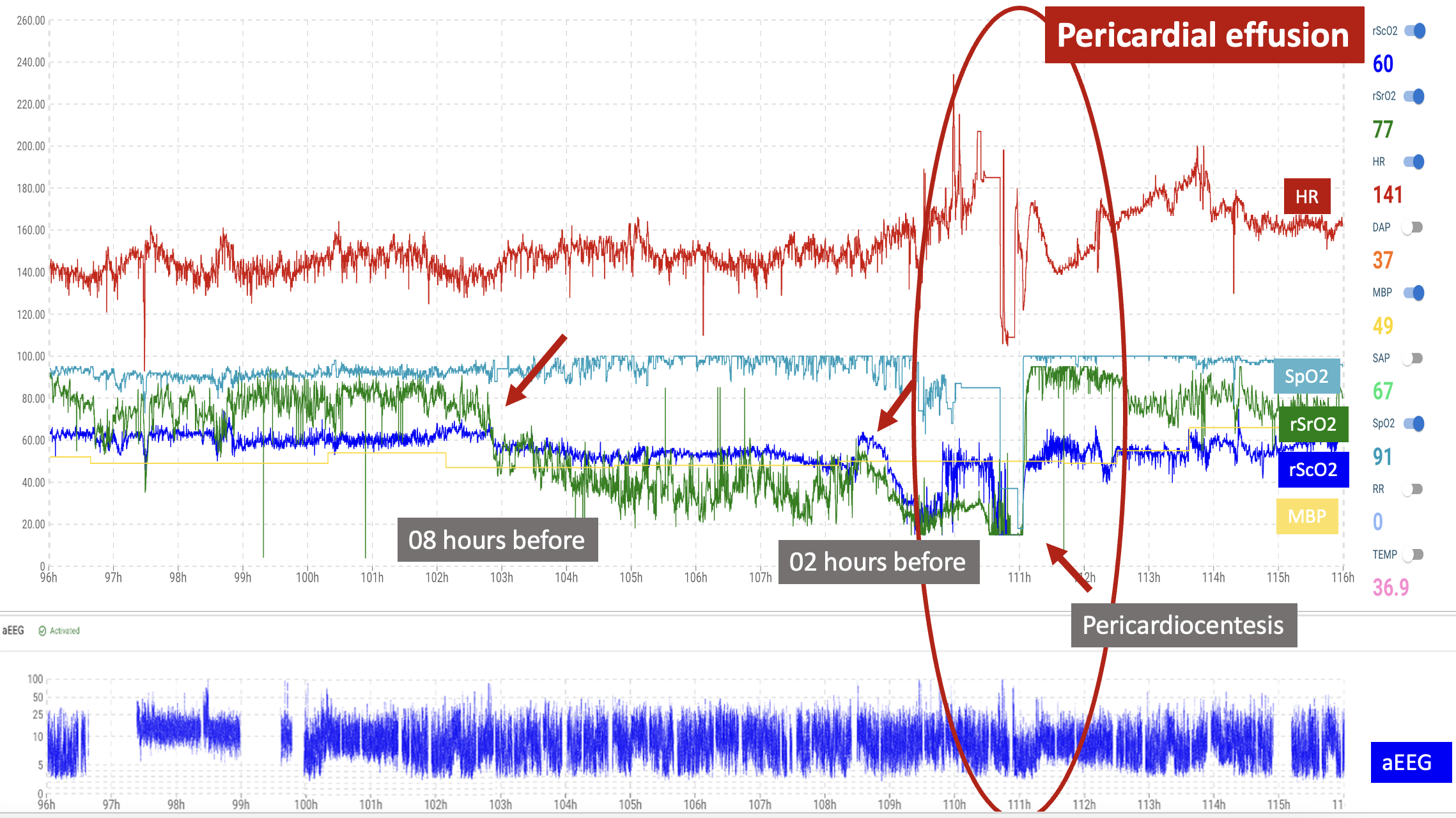
Case 2: A preterm with GA 29 weeks and BW 970g, was admitted to the NICU with respiratory distress and was stable on CPAP with FiO2 30%. During the 4th DOL his pulse oximetry (SpO2) dropped to 20% and HR decreased from ~160bpm to ~100bpm. The rScO2 and rSrO2 were noted to trend downward two and eight hours, respectively, earlier than other vital signs abnormalities. The infant was diagnosed with a pericardial effusion by cardiac echo. After pericardiocentesis a recovery of SpO2, HR, rScO2 and rSrO2 was immediately seen (Figure 2).
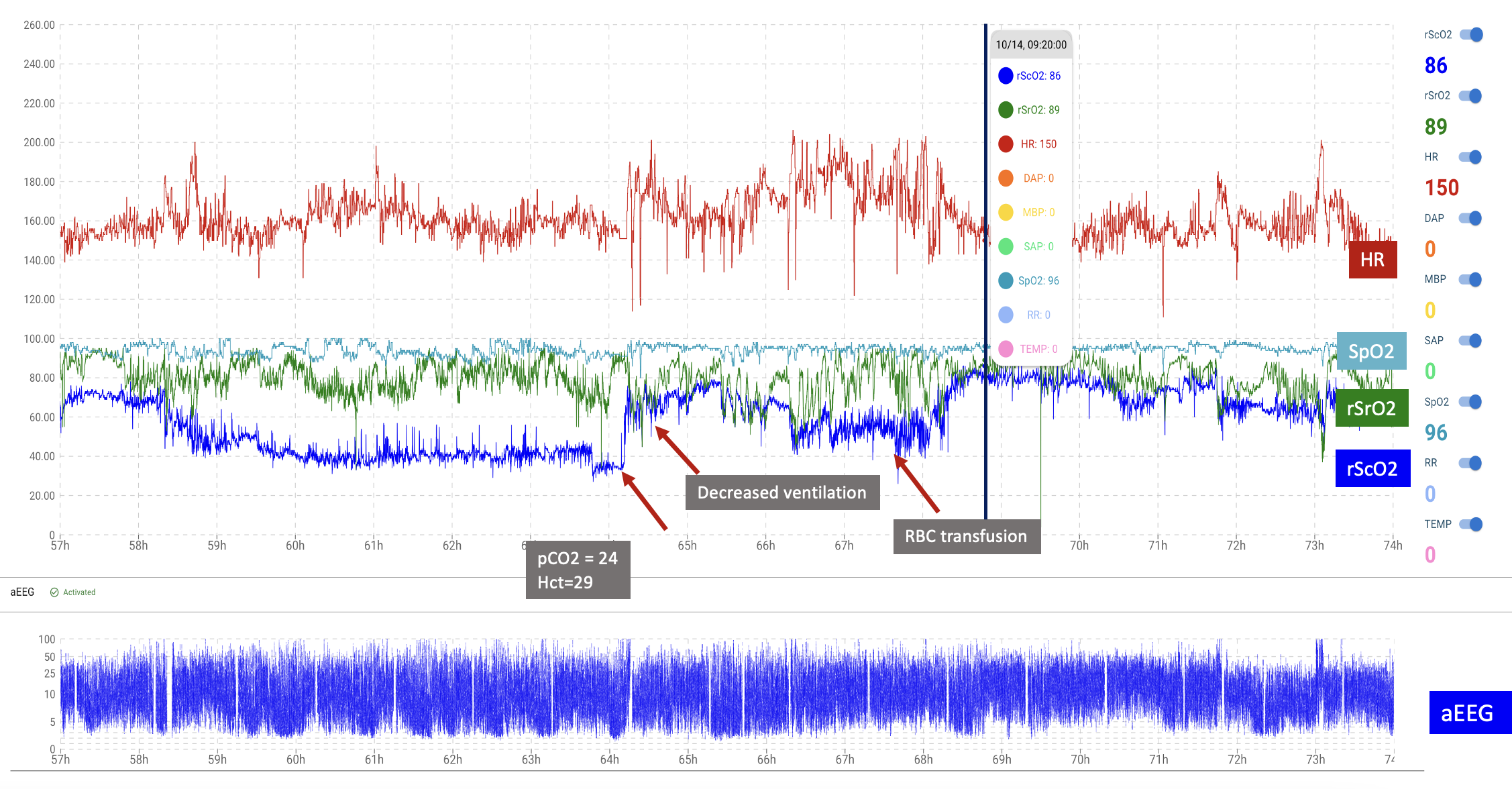
Case 3: A preterm with GA 28 weeks, BW 1080g, was admitted to the NICU and required intubation due to respiratory distress syndrome. On the 3rd DOL, a decrease in rScO2 from ~65% to ~35% was noted. Blood gas and hematocrit (Hct) were collected and identified hypocarbia (pCO2=24mmHg) and anemia (Hct=29). After ventilator adjustments and red blood cell transfusion, the rScO2 increased steadily to the normal range (Figure 3).
Conclusion(s): As neurocritical care has become a significant focus in the NICU, aEEG, NIRS and other traditionally used vital signs have shown utility in a population of babies at high risk for brain injury as exemplified in these clinical scenarios. We propose that routine combined analysis of these parameters may become the future standard for neonatal monitoring.